Sunday Poster Session
Category: Liver
P1231 - The Role of Sex in the Efficacy of Radical Surgical Resection of Hepatocellular Carcinoma: A Retrospective Analysis of the Surveillance Epidemiology and End Results Database
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- OB
Olivia Biernacki
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Olivia Biernacki, 1, Samuel Kim, BA1, Praneet Khanna, BA1, Mahi Gangavarapu, BA1, Akhila Swarna, 1, Bianca Ituarte, BA1, Islam Mohamed, MD2
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri, Columbia, MO
Introduction: Hepatocellular carcinoma (HCC) is the fourth leading cause of cancer-related mortality worldwide, with rising incidence and mortality rates observed over the past two decades. Previous epidemiological studies have identified possible treatment options including chemotherapy, immunotherapy, the use of oncolytic viruses, or a combination of these methods. Despite the availability of various treatment options, high mortality rates for HCC patients indicate the absence of a universally efficacious treatment. Investigating the influence of sex on the efficacy of radical surgical resection for HCC holds potential significance in understanding sex-based disparities in treatment. This study aims to describe survival rates following radical surgical resection for HCC among male and female patients to identify opportunities for tailored treatment approaches in patients.
Methods: Demographic and clinical data of patients with microscopically confirmed HCC were extracted from the Surveillance Epidemiology and End Results (SEER) database. The SEER registries included in our study included 17 cancer registries between the years 2000-2020. Cases were identified using the International Classification of Diseases (ICD) for Oncology, Third Revision morphology codes (8170-8175, 8180), localized to the liver (Primary Site: CXX.X-XX.Y). Cox proportional hazards model and Kaplan Meier curves (KM) have been used to describe survival, with significance assigned at p< 0.05.
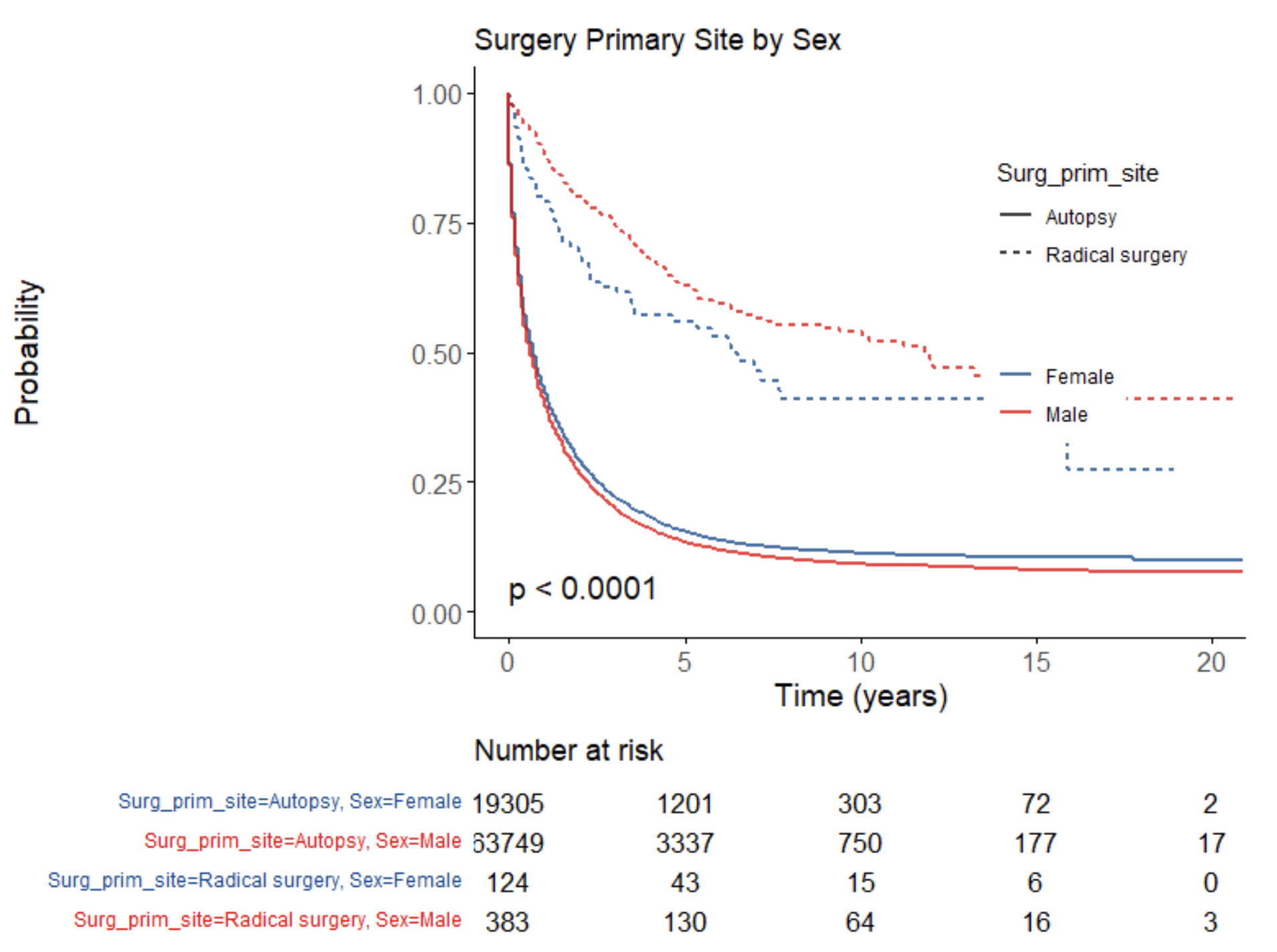
Results: A total of 110, 505 patients were included in this study. 76.1% of patients were male (n = 84, 089). Few patients received radical surgery (n = 607). With no surgery, males had a 7% increased risk of death (p < 0.001). With radical surgery, males had a 29% decreased risk of death compared to females (p = 0.007). KM curves confirm better overall survival (OS) when males receive radical surgery compared to females (p < 0.0001). KM curves also confirm worse OS when no surgery was pursued (p < 0.0001) as seen in Figure 1.
Discussion: This investigation found that radical surgery had a statistically significant decrease in risk of death for males compared to females. Despite this, previous studies have established better OS for females than males. Although this study is limited by the retrospective design, the investigation demonstrates that certain therapeutic courses may benefit males more than females. Future research is required to elucidate better therapeutic algorithms for different demographic groups.
Disclosures:
Olivia Biernacki, 1, Samuel Kim, BA1, Praneet Khanna, BA1, Mahi Gangavarapu, BA1, Akhila Swarna, 1, Bianca Ituarte, BA1, Islam Mohamed, MD2. P1231 - The Role of Sex in the Efficacy of Radical Surgical Resection of Hepatocellular Carcinoma: A Retrospective Analysis of the Surveillance Epidemiology and End Results Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri, Columbia, MO
Introduction: Hepatocellular carcinoma (HCC) is the fourth leading cause of cancer-related mortality worldwide, with rising incidence and mortality rates observed over the past two decades. Previous epidemiological studies have identified possible treatment options including chemotherapy, immunotherapy, the use of oncolytic viruses, or a combination of these methods. Despite the availability of various treatment options, high mortality rates for HCC patients indicate the absence of a universally efficacious treatment. Investigating the influence of sex on the efficacy of radical surgical resection for HCC holds potential significance in understanding sex-based disparities in treatment. This study aims to describe survival rates following radical surgical resection for HCC among male and female patients to identify opportunities for tailored treatment approaches in patients.
Methods: Demographic and clinical data of patients with microscopically confirmed HCC were extracted from the Surveillance Epidemiology and End Results (SEER) database. The SEER registries included in our study included 17 cancer registries between the years 2000-2020. Cases were identified using the International Classification of Diseases (ICD) for Oncology, Third Revision morphology codes (8170-8175, 8180), localized to the liver (Primary Site: CXX.X-XX.Y). Cox proportional hazards model and Kaplan Meier curves (KM) have been used to describe survival, with significance assigned at p< 0.05.
Results: A total of 110, 505 patients were included in this study. 76.1% of patients were male (n = 84, 089). Few patients received radical surgery (n = 607). With no surgery, males had a 7% increased risk of death (p < 0.001). With radical surgery, males had a 29% decreased risk of death compared to females (p = 0.007). KM curves confirm better overall survival (OS) when males receive radical surgery compared to females (p < 0.0001). KM curves also confirm worse OS when no surgery was pursued (p < 0.0001) as seen in Figure 1.
Discussion: This investigation found that radical surgery had a statistically significant decrease in risk of death for males compared to females. Despite this, previous studies have established better OS for females than males. Although this study is limited by the retrospective design, the investigation demonstrates that certain therapeutic courses may benefit males more than females. Future research is required to elucidate better therapeutic algorithms for different demographic groups.
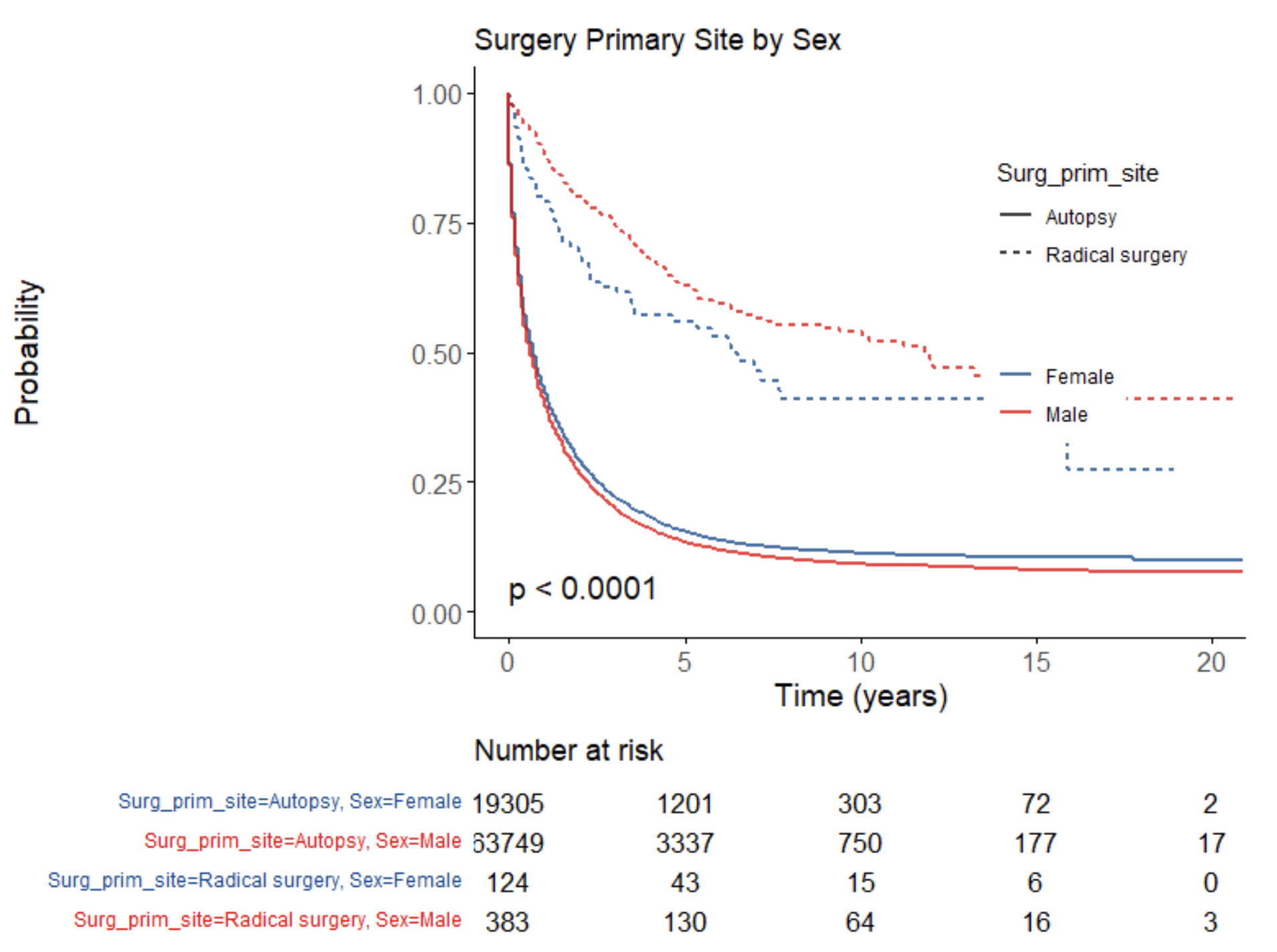
Figure: Figure 1. Kaplan Meier curves for overall survival by radical surgery and sex demonstrate better survival for males compared to females. The Kaplan Meier curves demonstrate worse overall prognosis for males when no surgery was pursued (autopsy).
Disclosures:
Olivia Biernacki indicated no relevant financial relationships.
Samuel Kim indicated no relevant financial relationships.
Praneet Khanna indicated no relevant financial relationships.
Mahi Gangavarapu indicated no relevant financial relationships.
Akhila Swarna indicated no relevant financial relationships.
Bianca Ituarte indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Olivia Biernacki, 1, Samuel Kim, BA1, Praneet Khanna, BA1, Mahi Gangavarapu, BA1, Akhila Swarna, 1, Bianca Ituarte, BA1, Islam Mohamed, MD2. P1231 - The Role of Sex in the Efficacy of Radical Surgical Resection of Hepatocellular Carcinoma: A Retrospective Analysis of the Surveillance Epidemiology and End Results Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
