Sunday Poster Session
Category: Liver
P1236 - Current Recommendations on Etiological Testing in Liver Cirrhosis: Is It Time for a Stepwise Approach?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Tanvi Gupta, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Tanvi Gupta, MD1, Sabiha Armin, MD1, Kazi Haque, MD2, Antonio Pizuorno Machado, MD, MPH3, Priscila Olague, MD4, Blake Purtle, MD5, Emily Leong, MD1, Evan Li, MD1, Emmanuel Luis A. Avelino, MD4, Yadier Brito-Cuas, MD1, Jennifer Ma, MD1, Kevin Chiu, MD1, Clay Smithhart, MD1, Stephen Glombicki, MD6, Gabriel Aisenberg, MD1
1University of Texas Health, McGovern Medical School, Houston, TX; 2McGovern Medical School at UTHealth, Pearland, TX; 3UT Southwstern Medical Center, Dallas, TX; 4University of Texas at Houston, Houston, TX; 5UT McGovern, Irving, TX; 6University of Texas, Houston, TX
Introduction: Cirrhosis represents a significant global health challenge, contributing to millions of deaths annually. Current guidelines recommend that patients with cirrhosis should be investigated for all its etiologies, although the most common culprits are hepatitis C virus (HCV) or significant alcohol use (SAU). We aimed to determine the value of screening for other causes of cirrhosis in patient encounters where the most common etiologies are already known.
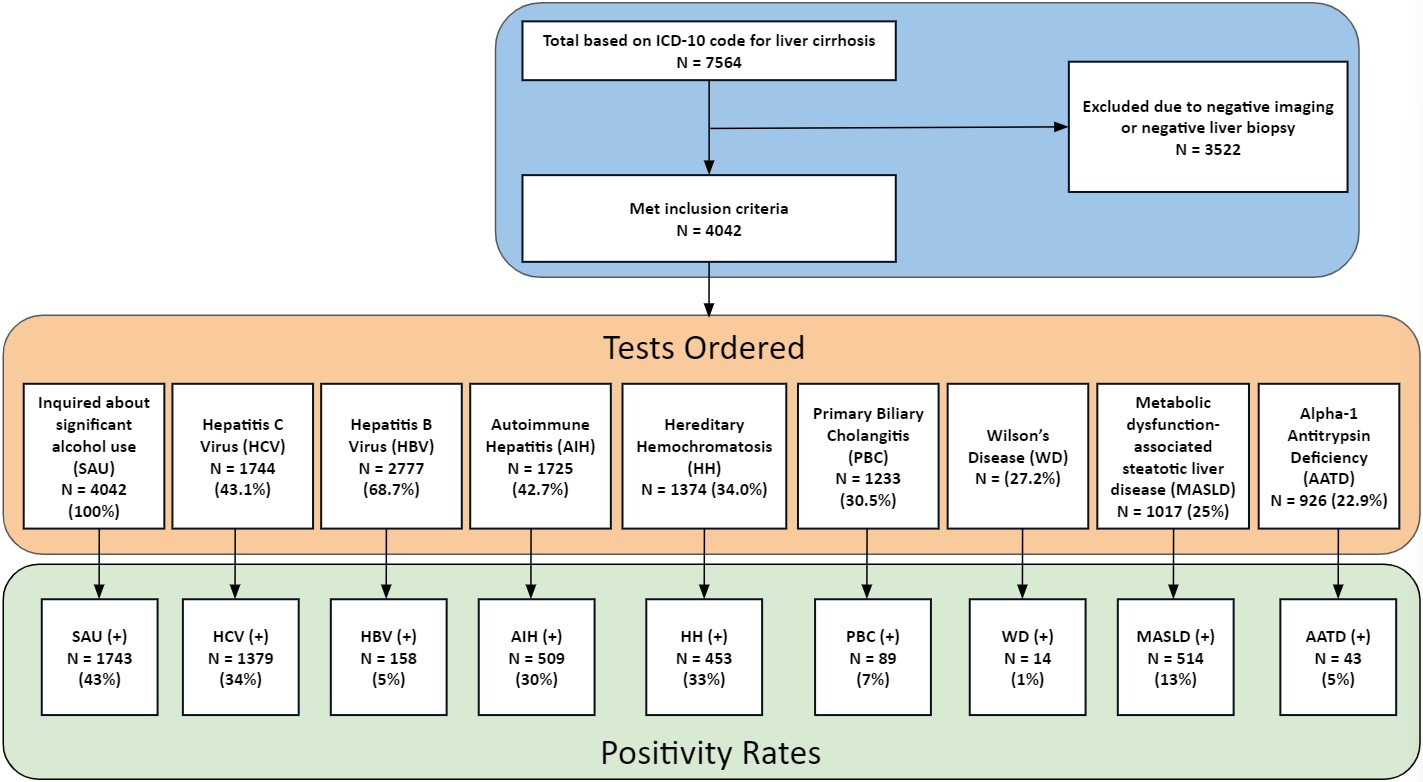
Methods: This was a retrospective study from 2015 to 2016 of adult patients diagnosed with cirrhosis, by ICD-10 codes, at a community hospital, a level 1 trauma center, and other surrounding hospitals. Patients were included after positive imaging and/or biopsy for cirrhosis. Demographic data, Child Pugh scores at the time of the cirrhosis diagnosis, and data on etiologies including SAU, HCV, hepatitis B virus, hereditary hemochromatosis, autoimmune hepatitis, Wilson’s disease, alpha-1 antitrypsin deficiency, and metabolic dysfunction-associated steatotic liver disease were collected. Groups stratified by SAU, HCV, both and neither, were compared to assess positivity rates among other etiologies of cirrhosis. Statistical analysis was performed with P values < 0.05 deemed statistically significant.
Results: 4042 of 7564 patients met inclusion criteria. SAU was identified in 1743 (43%) patients, HCV in 1379 (34%), both SAU and HCV in 661 (16%), and neither in 1581 (39%). The majority were classified as Child Pugh Score B (49%). Overall, 28% of patients with only HCV tested positive for at least one additional diagnosis compared to the 39% of patients without HCV (p < 0.01). In patients with only SAU, 24% tested positive for at least one additional test compared to 41% without SAU (p < 0.01). Among the patients with HCV and SAU, 22% had at least one additional test positive versus 36% of positive tests without those diseases (p < 0.01).
Discussion: Patients with SAU and HCV significantly demonstrated a lower likelihood of testing positive for other causes of cirrhosis. Conversely, patients without SAU or HCV were significantly more likely to test positive for other etiologies. This suggests that in clinical settings where SAU or HCV are identified as the primary etiologies, additional diagnostic tests for alternative causes may offer limited clinical utility. We recommend a tailored stepwise approach to diagnostic testing, starting with SAU and HCV, followed by the other etiologies of cirrhosis, if clinically indicated.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tanvi Gupta, MD1, Sabiha Armin, MD1, Kazi Haque, MD2, Antonio Pizuorno Machado, MD, MPH3, Priscila Olague, MD4, Blake Purtle, MD5, Emily Leong, MD1, Evan Li, MD1, Emmanuel Luis A. Avelino, MD4, Yadier Brito-Cuas, MD1, Jennifer Ma, MD1, Kevin Chiu, MD1, Clay Smithhart, MD1, Stephen Glombicki, MD6, Gabriel Aisenberg, MD1. P1236 - Current Recommendations on Etiological Testing in Liver Cirrhosis: Is It Time for a Stepwise Approach?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2McGovern Medical School at UTHealth, Pearland, TX; 3UT Southwstern Medical Center, Dallas, TX; 4University of Texas at Houston, Houston, TX; 5UT McGovern, Irving, TX; 6University of Texas, Houston, TX
Introduction: Cirrhosis represents a significant global health challenge, contributing to millions of deaths annually. Current guidelines recommend that patients with cirrhosis should be investigated for all its etiologies, although the most common culprits are hepatitis C virus (HCV) or significant alcohol use (SAU). We aimed to determine the value of screening for other causes of cirrhosis in patient encounters where the most common etiologies are already known.
Methods: This was a retrospective study from 2015 to 2016 of adult patients diagnosed with cirrhosis, by ICD-10 codes, at a community hospital, a level 1 trauma center, and other surrounding hospitals. Patients were included after positive imaging and/or biopsy for cirrhosis. Demographic data, Child Pugh scores at the time of the cirrhosis diagnosis, and data on etiologies including SAU, HCV, hepatitis B virus, hereditary hemochromatosis, autoimmune hepatitis, Wilson’s disease, alpha-1 antitrypsin deficiency, and metabolic dysfunction-associated steatotic liver disease were collected. Groups stratified by SAU, HCV, both and neither, were compared to assess positivity rates among other etiologies of cirrhosis. Statistical analysis was performed with P values < 0.05 deemed statistically significant.
Results: 4042 of 7564 patients met inclusion criteria. SAU was identified in 1743 (43%) patients, HCV in 1379 (34%), both SAU and HCV in 661 (16%), and neither in 1581 (39%). The majority were classified as Child Pugh Score B (49%). Overall, 28% of patients with only HCV tested positive for at least one additional diagnosis compared to the 39% of patients without HCV (p < 0.01). In patients with only SAU, 24% tested positive for at least one additional test compared to 41% without SAU (p < 0.01). Among the patients with HCV and SAU, 22% had at least one additional test positive versus 36% of positive tests without those diseases (p < 0.01).
Discussion: Patients with SAU and HCV significantly demonstrated a lower likelihood of testing positive for other causes of cirrhosis. Conversely, patients without SAU or HCV were significantly more likely to test positive for other etiologies. This suggests that in clinical settings where SAU or HCV are identified as the primary etiologies, additional diagnostic tests for alternative causes may offer limited clinical utility. We recommend a tailored stepwise approach to diagnostic testing, starting with SAU and HCV, followed by the other etiologies of cirrhosis, if clinically indicated.
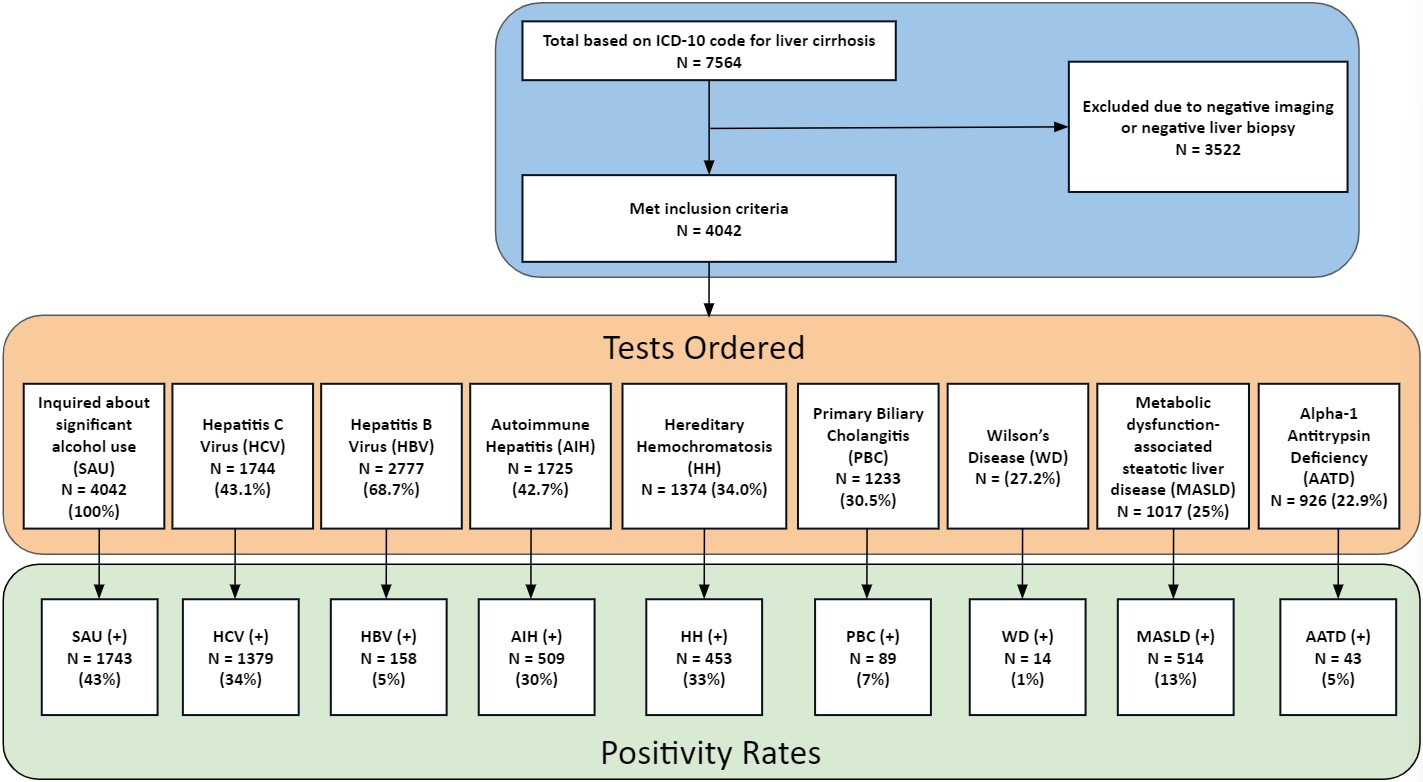
Figure: Figure 1: Flow diagram for study participants, including the names of each test/etiology of cirrhosis and their respective positivity rates
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tanvi Gupta indicated no relevant financial relationships.
Sabiha Armin indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Antonio Pizuorno Machado indicated no relevant financial relationships.
Priscila Olague indicated no relevant financial relationships.
Blake Purtle indicated no relevant financial relationships.
Emily Leong indicated no relevant financial relationships.
Evan Li indicated no relevant financial relationships.
Emmanuel Luis Avelino indicated no relevant financial relationships.
Yadier Brito-Cuas indicated no relevant financial relationships.
Jennifer Ma indicated no relevant financial relationships.
Kevin Chiu indicated no relevant financial relationships.
Clay Smithhart indicated no relevant financial relationships.
Stephen Glombicki indicated no relevant financial relationships.
Gabriel Aisenberg indicated no relevant financial relationships.
Tanvi Gupta, MD1, Sabiha Armin, MD1, Kazi Haque, MD2, Antonio Pizuorno Machado, MD, MPH3, Priscila Olague, MD4, Blake Purtle, MD5, Emily Leong, MD1, Evan Li, MD1, Emmanuel Luis A. Avelino, MD4, Yadier Brito-Cuas, MD1, Jennifer Ma, MD1, Kevin Chiu, MD1, Clay Smithhart, MD1, Stephen Glombicki, MD6, Gabriel Aisenberg, MD1. P1236 - Current Recommendations on Etiological Testing in Liver Cirrhosis: Is It Time for a Stepwise Approach?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

