Sunday Poster Session
Category: Liver
P1239 - Clinical and Demographic Disparities in Patients With Overlapping Autoimmune Hepatitis and Systemic Lupus Erythematosus: A Comprehensive Nationwide Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SP
Sreeram Pannala, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2, Liliane Deeb, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Southern Illinois University, Springfield, IL
Introduction: Liver involvement is not uncommon in patients with systemic lupus erythematosus (SLE). This could result from lupus hepatitis, drug-induced hepatotoxicity, or concomitant liver disorders. Multiple case reports suggested an overlap between autoimmune hepatitis (AIH) and SLE, in a way AIH may develop during the course of SLE or as a primary manifestation. Our study primarily focuses on evaluating the overlap between AIH and SLE.
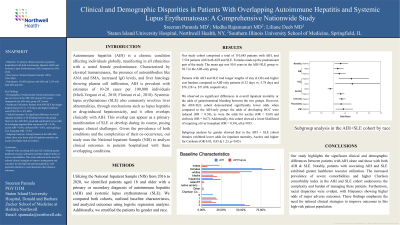
Methods: Utilizing the National Inpatient Sample (NIS) from 2016 to 2020, we identified patients older than 18, with a primary or secondary diagnosis of AIH and SLE. We compared both cohorts, outlined baseline characteristics, and analyzed outcomes using logistic regression analysis. Additionally, we stratified the patients by gender & race.
Results: Adjusted odds for HCC in AIH+SLE were lower (OR 0.38), but Hispanics showed increased odds (OR 1.76) (p< 0.05). For Ascites, the AIH+SLE cohort had lower adjusted odds (OR 0.69); females and Blacks also had lower odds (OR 0.85 and 0.87), while Hispanics had higher (OR 1.31) (p< 0.05). Adjusted odds for developing cirrhosis in the AIH+SLE cohort were 0.67, with females and Hispanics having higher odds (OR 1.23 and 1.36) (p< 0.05). Hispanics in the AIH+SLE cohort had higher odds of pancreatitis (OR 1.33) & sepsis (OR 1.16)(p< 0.05). Blacks & Hispanics had higher odds of GI bleeding in AIH+SLE (OR 1.19 & 1.25) (p< 0.05). The odds of needing a liver transplant were lower in AIH+SLE compared to AIH (OR 0.39), but Hispanics had higher odds (OR 1.42) (p< 0.05). In AIH+SLE, Hispanics had higher odds for portal venous thrombosis (OR 1.74) while Blacks had lower odds (OR 0.67) (p< 0.05). Overall inpatient mortality wasn't significantly different, but in AIH+SLE, Hispanics had higher inpatient mortality odds (OR 1.31) (p< 0.05). AIH+SLE patients had longer stays and higher costs than AIH patients (6.32 days vs. 5.78 days; $76,128 vs. $71,688).
Discussion: Our study highlights the significant clinical and demographic differences between patients with isolated AIH and those with concomitant AIH & SLE. Patients with AIH+SLE exhibited greater healthcare resource utilization. Furthermore, racial disparities were evident, with Hispanics showing higher odds of adverse outcomes such as GI bleeding, HCC, PVT, and Liver transplant. These findings emphasize the need for tailored clinical strategies to improve outcomes in this high-risk population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2, Liliane Deeb, MD1. P1239 - Clinical and Demographic Disparities in Patients With Overlapping Autoimmune Hepatitis and Systemic Lupus Erythematosus: A Comprehensive Nationwide Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Southern Illinois University, Springfield, IL
Introduction: Liver involvement is not uncommon in patients with systemic lupus erythematosus (SLE). This could result from lupus hepatitis, drug-induced hepatotoxicity, or concomitant liver disorders. Multiple case reports suggested an overlap between autoimmune hepatitis (AIH) and SLE, in a way AIH may develop during the course of SLE or as a primary manifestation. Our study primarily focuses on evaluating the overlap between AIH and SLE.
Methods: Utilizing the National Inpatient Sample (NIS) from 2016 to 2020, we identified patients older than 18, with a primary or secondary diagnosis of AIH and SLE. We compared both cohorts, outlined baseline characteristics, and analyzed outcomes using logistic regression analysis. Additionally, we stratified the patients by gender & race.
Results: Adjusted odds for HCC in AIH+SLE were lower (OR 0.38), but Hispanics showed increased odds (OR 1.76) (p< 0.05). For Ascites, the AIH+SLE cohort had lower adjusted odds (OR 0.69); females and Blacks also had lower odds (OR 0.85 and 0.87), while Hispanics had higher (OR 1.31) (p< 0.05). Adjusted odds for developing cirrhosis in the AIH+SLE cohort were 0.67, with females and Hispanics having higher odds (OR 1.23 and 1.36) (p< 0.05). Hispanics in the AIH+SLE cohort had higher odds of pancreatitis (OR 1.33) & sepsis (OR 1.16)(p< 0.05). Blacks & Hispanics had higher odds of GI bleeding in AIH+SLE (OR 1.19 & 1.25) (p< 0.05). The odds of needing a liver transplant were lower in AIH+SLE compared to AIH (OR 0.39), but Hispanics had higher odds (OR 1.42) (p< 0.05). In AIH+SLE, Hispanics had higher odds for portal venous thrombosis (OR 1.74) while Blacks had lower odds (OR 0.67) (p< 0.05). Overall inpatient mortality wasn't significantly different, but in AIH+SLE, Hispanics had higher inpatient mortality odds (OR 1.31) (p< 0.05). AIH+SLE patients had longer stays and higher costs than AIH patients (6.32 days vs. 5.78 days; $76,128 vs. $71,688).
Discussion: Our study highlights the significant clinical and demographic differences between patients with isolated AIH and those with concomitant AIH & SLE. Patients with AIH+SLE exhibited greater healthcare resource utilization. Furthermore, racial disparities were evident, with Hispanics showing higher odds of adverse outcomes such as GI bleeding, HCC, PVT, and Liver transplant. These findings emphasize the need for tailored clinical strategies to improve outcomes in this high-risk population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Medha Rajamanuri indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2, Liliane Deeb, MD1. P1239 - Clinical and Demographic Disparities in Patients With Overlapping Autoimmune Hepatitis and Systemic Lupus Erythematosus: A Comprehensive Nationwide Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
