Sunday Poster Session
Category: Liver
P1178 - Evaluating and Improving the Use of Nutritional Interventions in Hospitalized Patients With Cirrhosis: A Quality Improvement Project.
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Avneet Singh, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Avneet Singh, DO1, Alexander Garcia, DO1, Nicole Debski, BS2, Erin Sanzone, BS2, Alexis Sieber, BS2, Krystal Hunter, PhD, MBA3, Jason Ho, MD4, Kathy N. Williams, MD, MS5, Christopher Deitch, MD4
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper University Health Care, Camden, NJ; 4Cooper Health Gastroenterology, Camden, NJ; 5Cooper University Hospital, Philadelphia, PA
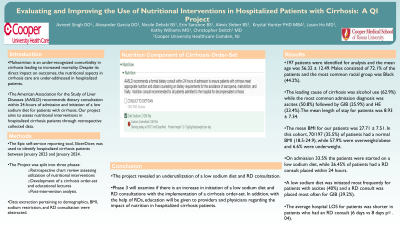
Introduction: Malnutrition is an under-recognized comorbidity in cirrhosis leading to increased mortality. Despite its direct impact on outcomes, the nutritional aspects in cirrhosis care are under-addressed in hospitalized patients. The American Association for the Study of Liver Diseases (AASLD) recommends dietary consultation within 24-hours of admission and initiation of a low sodium diet for patients with cirrhosis. Our project aims to assess nutritional interventions in hospitalized cirrhosis patients through retrospective collected data.
Methods: The project was split into three phases: 1) retrospective chart review assessing utilization of nutritional intervention, 2) development of a cirrhosis order-set and educational lectures and 3) post-intervention analysis. The Epic self-service reporting tool, SlicerDicer, was used to identify hospitalized cirrhosis patients between January 2023 and January 2024. Patients were then sub-categorized into three groups; hepatic encephalopathy (HE), ascites, or gastrointestinal bleed (GIB). Data extraction pertaining to demographics, BMI, sodium restriction, and RD consultation were abstracted.
Results: 197 patients were identified with a mean age of 56.32 ± 12.49 and mean length of stay of 8.93 ± 7.34. The mean BMI was 27.71 ± 7.51 and 70/197 (35.5%) of patients had a normal BMI (18.5-24.9), while 57.9% were overweight/obese and 6.6% underweight. Male (72.1%) patients exceeded females (27.9%). Majority of patients were Black (44.2%) and the leading cause of cirrhosis was alcohol use (62.9%). The most common admission diagnosis was ascites (50.8%) followed by GIB (25.9%) and HE (23.4%). At admission 66/197 (33.5%) of the patients were started on a low sodium diet, while 52/197 (26.45%) had a RD consult placed within 24 hours. Stratified by diagnosis, a low sodium diet was initiated most frequently for ascites (40%) and a RD consult was placed most often for GIB (39.2%). The average hospital length of stay for patients was significantly shorter in patients who had an RD consult compared to those who did not (6 days vs 8 days p= .04).
Discussion: Our QI project revealed there was an underutilization of a low sodium diet and RD consultation. Phase 3 will examine if there is an increase in initiation of a low sodium diet and RD consultations with the implementation of a cirrhosis order-set. In addition, with the help of RDs, education will be given to providers and physicians regarding the impact of nutrition in hospitalized cirrhosis patients.
Disclosures:
Avneet Singh, DO1, Alexander Garcia, DO1, Nicole Debski, BS2, Erin Sanzone, BS2, Alexis Sieber, BS2, Krystal Hunter, PhD, MBA3, Jason Ho, MD4, Kathy N. Williams, MD, MS5, Christopher Deitch, MD4. P1178 - Evaluating and Improving the Use of Nutritional Interventions in Hospitalized Patients With Cirrhosis: A Quality Improvement Project., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper University Health Care, Camden, NJ; 4Cooper Health Gastroenterology, Camden, NJ; 5Cooper University Hospital, Philadelphia, PA
Introduction: Malnutrition is an under-recognized comorbidity in cirrhosis leading to increased mortality. Despite its direct impact on outcomes, the nutritional aspects in cirrhosis care are under-addressed in hospitalized patients. The American Association for the Study of Liver Diseases (AASLD) recommends dietary consultation within 24-hours of admission and initiation of a low sodium diet for patients with cirrhosis. Our project aims to assess nutritional interventions in hospitalized cirrhosis patients through retrospective collected data.
Methods: The project was split into three phases: 1) retrospective chart review assessing utilization of nutritional intervention, 2) development of a cirrhosis order-set and educational lectures and 3) post-intervention analysis. The Epic self-service reporting tool, SlicerDicer, was used to identify hospitalized cirrhosis patients between January 2023 and January 2024. Patients were then sub-categorized into three groups; hepatic encephalopathy (HE), ascites, or gastrointestinal bleed (GIB). Data extraction pertaining to demographics, BMI, sodium restriction, and RD consultation were abstracted.
Results: 197 patients were identified with a mean age of 56.32 ± 12.49 and mean length of stay of 8.93 ± 7.34. The mean BMI was 27.71 ± 7.51 and 70/197 (35.5%) of patients had a normal BMI (18.5-24.9), while 57.9% were overweight/obese and 6.6% underweight. Male (72.1%) patients exceeded females (27.9%). Majority of patients were Black (44.2%) and the leading cause of cirrhosis was alcohol use (62.9%). The most common admission diagnosis was ascites (50.8%) followed by GIB (25.9%) and HE (23.4%). At admission 66/197 (33.5%) of the patients were started on a low sodium diet, while 52/197 (26.45%) had a RD consult placed within 24 hours. Stratified by diagnosis, a low sodium diet was initiated most frequently for ascites (40%) and a RD consult was placed most often for GIB (39.2%). The average hospital length of stay for patients was significantly shorter in patients who had an RD consult compared to those who did not (6 days vs 8 days p= .04).
Discussion: Our QI project revealed there was an underutilization of a low sodium diet and RD consultation. Phase 3 will examine if there is an increase in initiation of a low sodium diet and RD consultations with the implementation of a cirrhosis order-set. In addition, with the help of RDs, education will be given to providers and physicians regarding the impact of nutrition in hospitalized cirrhosis patients.
Disclosures:
Avneet Singh indicated no relevant financial relationships.
Alexander Garcia indicated no relevant financial relationships.
Nicole Debski indicated no relevant financial relationships.
Erin Sanzone indicated no relevant financial relationships.
Alexis Sieber indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Jason Ho indicated no relevant financial relationships.
Kathy Williams indicated no relevant financial relationships.
Christopher Deitch indicated no relevant financial relationships.
Avneet Singh, DO1, Alexander Garcia, DO1, Nicole Debski, BS2, Erin Sanzone, BS2, Alexis Sieber, BS2, Krystal Hunter, PhD, MBA3, Jason Ho, MD4, Kathy N. Williams, MD, MS5, Christopher Deitch, MD4. P1178 - Evaluating and Improving the Use of Nutritional Interventions in Hospitalized Patients With Cirrhosis: A Quality Improvement Project., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

