Sunday Poster Session
Category: Interventional Endoscopy
P1084 - A Rare Presentation of Bateman Purpura Following ERCP
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kathryn Welp, MD
Vanderbilt University Medical Center
Nashville, TN
Presenting Author(s)
Award: Presidential Poster Award
Kathryn Welp, MD, Ananya Sharma, MD, Claudio Tombazzi, MD, Mark Radlinski, MD
Vanderbilt University Medical Center, Nashville, TN
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) has known adverse events including pancreatitis, infection, hemorrhage, and perforation. Rarely, ERCP can cause microvascular complications concerning for acute hemolytic and thrombotic processes. Here we highlight Bateman purpura (BP), a rare complication of ERCP.
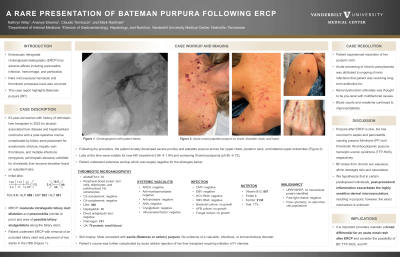
Case Description/Methods: A 63-year-old woman with history of orthotopic liver transplant in 2023 for alcohol-associated liver disease and hepatocellular carcinoma with a post-operative course complicated by biliary stent placement for anastomotic stricture and multiple infections (empyema, peri-hepatic abscess) requiring chronic antibiotic therapy was admitted for cholestatic liver enzyme elevation. She subsequently underwent ERCP with removal of an occluded biliary stent and placement of two stents in the common bile duct. Following the procedure, she acutely developed severe pruritus and palpable purpura across her upper chest, posterior neck, and bilateral upper extremities (Figure 1) with lab derangements most notable for acute kidney injury and worsened thrombocytopenia. She underwent an extensive work-up that was negative for nutritional deficiencies, infectious etiologies, systemic vasculitis, and thrombotic microangiopathies. Ultimately, skin biopsy demonstrated BP. Renal dysfunction was attributed to peri-procedural AKI and thrombocytopenia was thought to be multifactorial involving medication side effects and bone marrow suppression from her pro-inflammatory state. Hospitalization was further complicated by moderate acute cellular rejection demonstrated on liver biopsy and the patient received intravenous steroids. Upon time of discharge, pruritus had greatly improved with supportive measures and rash remained stable.
Discussion: Purpura after ERCP is a rare phenomenon but has occurred in pancreatitis and sepsis, causing thrombotic thrombocytopenic purpura-hemolytic uremic syndrome (TTP-HUS) and purpura fulminans (PF), respectively. Compared to TTP-HUS and PF, BP, also known as actinic or senile purpura, is more benign and arises from chronic sun exposure which damages skin and vasculature. Though the exact mechanism is unknown, we hypothesize that in certain predisposed individuals, post-procedural inflammation exacerbates the highly sensitive dermal microvasculature resulting in blood extravasation and development of purpura. It is important providers are aware of the possibility of BP while maintaining a broad differential for an acute onset rash after ERCP.

Disclosures:
Kathryn Welp, MD, Ananya Sharma, MD, Claudio Tombazzi, MD, Mark Radlinski, MD. P1084 - A Rare Presentation of Bateman Purpura Following ERCP, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kathryn Welp, MD, Ananya Sharma, MD, Claudio Tombazzi, MD, Mark Radlinski, MD
Vanderbilt University Medical Center, Nashville, TN
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) has known adverse events including pancreatitis, infection, hemorrhage, and perforation. Rarely, ERCP can cause microvascular complications concerning for acute hemolytic and thrombotic processes. Here we highlight Bateman purpura (BP), a rare complication of ERCP.
Case Description/Methods: A 63-year-old woman with history of orthotopic liver transplant in 2023 for alcohol-associated liver disease and hepatocellular carcinoma with a post-operative course complicated by biliary stent placement for anastomotic stricture and multiple infections (empyema, peri-hepatic abscess) requiring chronic antibiotic therapy was admitted for cholestatic liver enzyme elevation. She subsequently underwent ERCP with removal of an occluded biliary stent and placement of two stents in the common bile duct. Following the procedure, she acutely developed severe pruritus and palpable purpura across her upper chest, posterior neck, and bilateral upper extremities (Figure 1) with lab derangements most notable for acute kidney injury and worsened thrombocytopenia. She underwent an extensive work-up that was negative for nutritional deficiencies, infectious etiologies, systemic vasculitis, and thrombotic microangiopathies. Ultimately, skin biopsy demonstrated BP. Renal dysfunction was attributed to peri-procedural AKI and thrombocytopenia was thought to be multifactorial involving medication side effects and bone marrow suppression from her pro-inflammatory state. Hospitalization was further complicated by moderate acute cellular rejection demonstrated on liver biopsy and the patient received intravenous steroids. Upon time of discharge, pruritus had greatly improved with supportive measures and rash remained stable.
Discussion: Purpura after ERCP is a rare phenomenon but has occurred in pancreatitis and sepsis, causing thrombotic thrombocytopenic purpura-hemolytic uremic syndrome (TTP-HUS) and purpura fulminans (PF), respectively. Compared to TTP-HUS and PF, BP, also known as actinic or senile purpura, is more benign and arises from chronic sun exposure which damages skin and vasculature. Though the exact mechanism is unknown, we hypothesize that in certain predisposed individuals, post-procedural inflammation exacerbates the highly sensitive dermal microvasculature resulting in blood extravasation and development of purpura. It is important providers are aware of the possibility of BP while maintaining a broad differential for an acute onset rash after ERCP.

Figure: Acute onset palpable purpura after ERCP on (A) chest, (B) shoulder, (C) back, and (D) hand.
Disclosures:
Kathryn Welp indicated no relevant financial relationships.
Ananya Sharma indicated no relevant financial relationships.
Claudio Tombazzi indicated no relevant financial relationships.
Mark Radlinski indicated no relevant financial relationships.
Kathryn Welp, MD, Ananya Sharma, MD, Claudio Tombazzi, MD, Mark Radlinski, MD. P1084 - A Rare Presentation of Bateman Purpura Following ERCP, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


