Sunday Poster Session
Category: Interventional Endoscopy
P1089 - Multi-Tool Endoscopic Management of Recalcitrant Bleeding Duodenal Varices in Portal, Splenic and Superior Mesenteric Vein Thromboses
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JS
Jessica Sosio, DO
Indiana University School of Medicine
Evansville, IN
Presenting Author(s)
Jessica Sosio, DO1, Hani Shamseddeen, MD2, Niharika Samala, MD2, Umer Bhatti, MD2, Mohammad Al-Haddad, MD, FACG2
1Indiana University School of Medicine, Evansville, IN; 2Indiana University School of Medicine, Indianapolis, IN
Introduction: Bleeding duodenal varices are a rare and potentially life-threatening complication of decompensated cirrhosis. No gold-standard treatment exists, and multiple single endoscopic approaches have been described in the literature. We present the case of a bleeding duodenal varix treated endoscopically with a multistep approach.
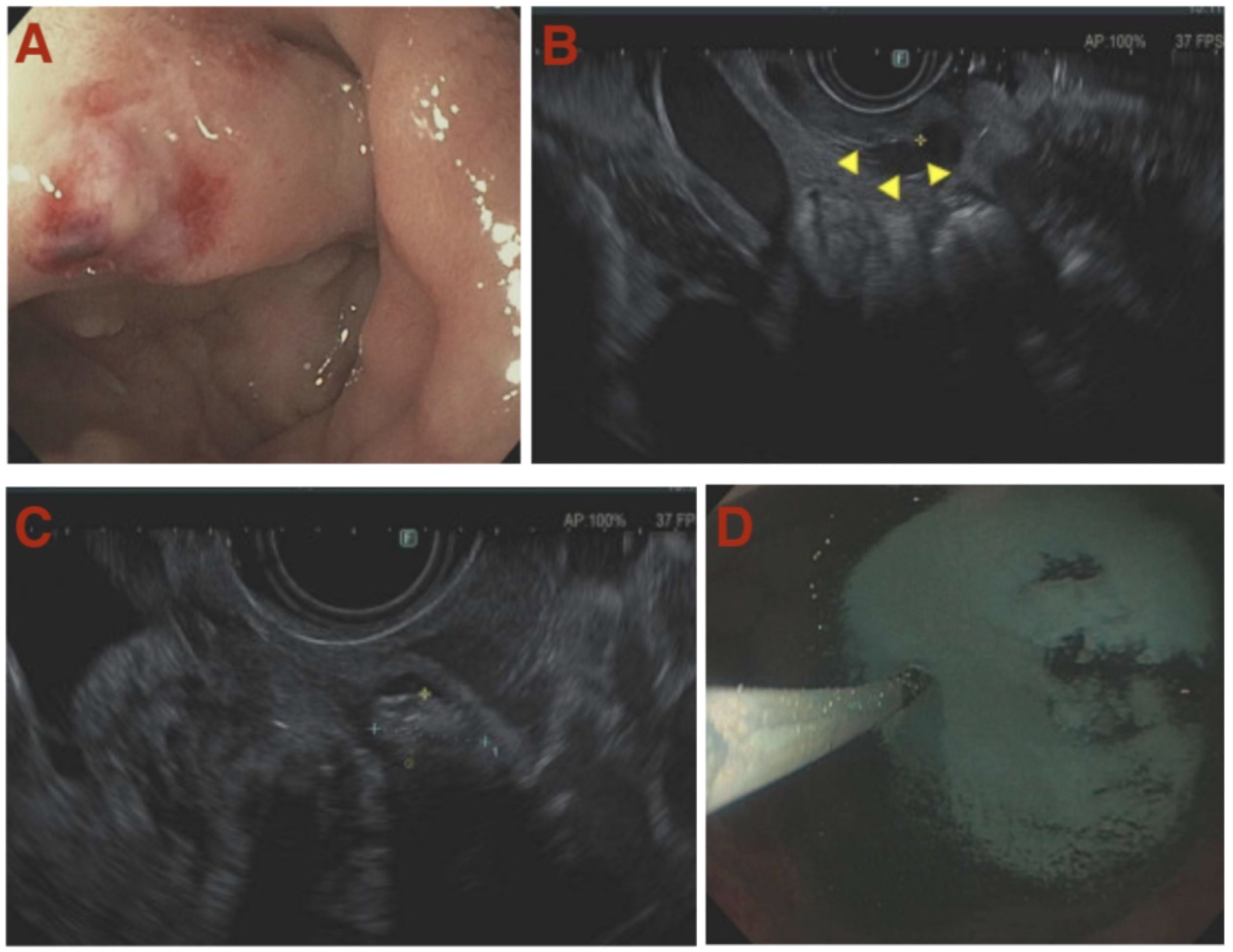
Case Description/Methods: A 41-year-old male with decompensated alcohol-associated cirrhosis, complicated by portal, splenic, and superior mesenteric vein thromboses, who received transjugular intrahepatic portosystemic shunt for gastric variceal bleeding complicated by shunt re-occlusion was hospitalized for bacteremia and candidemia while awaiting multivisceral transplantation (MVT). Earlier in the admission, he underwent esophagogastroduodenoscopy (EGD) for the placement of nasojejunal tube. During scope advancement, transient bleeding from what appeared to be a large duodenal varix was visualized in the first portion of the duodenum, which spontaneously stopped without any intervention. Computed tomography angiography showed no active bleeding, and he was taken to the endoscopy suite. Due to extensive splanchnic vein thrombosis, the varix was not accessible intravascularly by interventional radiology (IR). EGD revealed a grade II varix in the duodenal bulb with a red whale sign, and endoscopic ultrasound (EUS) showed multiple extensive duodenal varices, extending to D2 with the largest measuring 6 mm in diameter. EUS-guided sclerotherapy with cyanoacrylate was performed at the largest varix (Figure 1). However, due to persistent oozing, hemostatic powder was then used to successfully control the bleeding. The patient went on to receive MVT.
Discussion: Portal hypertension is a known complication of cirrhosis and the most common cause of portosystemic shunts and duodenal varices. Varices most commonly develop in the esophagus and stomach but can also be ectopic and occur in locations such as the duodenum. Duodenal varices are rare and difficult to diagnose, often leading to massive bleeding with a high rate of rebleeding and mortality. Bleeding duodenal varices can be managed endoscopically, surgically, or procedurally by IR. To date, no gold-standard treatment exists, and the choice of therapy depends on the facility and expertise available. Prior case reports have detailed single endoscopic approaches including sclerotherapy, banding, and the use of hemostatic powder but, to our knowledge, our case is the first to describe a stepwise escalation approach.
Disclosures:
Jessica Sosio, DO1, Hani Shamseddeen, MD2, Niharika Samala, MD2, Umer Bhatti, MD2, Mohammad Al-Haddad, MD, FACG2. P1089 - Multi-Tool Endoscopic Management of Recalcitrant Bleeding Duodenal Varices in Portal, Splenic and Superior Mesenteric Vein Thromboses, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Evansville, IN; 2Indiana University School of Medicine, Indianapolis, IN
Introduction: Bleeding duodenal varices are a rare and potentially life-threatening complication of decompensated cirrhosis. No gold-standard treatment exists, and multiple single endoscopic approaches have been described in the literature. We present the case of a bleeding duodenal varix treated endoscopically with a multistep approach.
Case Description/Methods: A 41-year-old male with decompensated alcohol-associated cirrhosis, complicated by portal, splenic, and superior mesenteric vein thromboses, who received transjugular intrahepatic portosystemic shunt for gastric variceal bleeding complicated by shunt re-occlusion was hospitalized for bacteremia and candidemia while awaiting multivisceral transplantation (MVT). Earlier in the admission, he underwent esophagogastroduodenoscopy (EGD) for the placement of nasojejunal tube. During scope advancement, transient bleeding from what appeared to be a large duodenal varix was visualized in the first portion of the duodenum, which spontaneously stopped without any intervention. Computed tomography angiography showed no active bleeding, and he was taken to the endoscopy suite. Due to extensive splanchnic vein thrombosis, the varix was not accessible intravascularly by interventional radiology (IR). EGD revealed a grade II varix in the duodenal bulb with a red whale sign, and endoscopic ultrasound (EUS) showed multiple extensive duodenal varices, extending to D2 with the largest measuring 6 mm in diameter. EUS-guided sclerotherapy with cyanoacrylate was performed at the largest varix (Figure 1). However, due to persistent oozing, hemostatic powder was then used to successfully control the bleeding. The patient went on to receive MVT.
Discussion: Portal hypertension is a known complication of cirrhosis and the most common cause of portosystemic shunts and duodenal varices. Varices most commonly develop in the esophagus and stomach but can also be ectopic and occur in locations such as the duodenum. Duodenal varices are rare and difficult to diagnose, often leading to massive bleeding with a high rate of rebleeding and mortality. Bleeding duodenal varices can be managed endoscopically, surgically, or procedurally by IR. To date, no gold-standard treatment exists, and the choice of therapy depends on the facility and expertise available. Prior case reports have detailed single endoscopic approaches including sclerotherapy, banding, and the use of hemostatic powder but, to our knowledge, our case is the first to describe a stepwise escalation approach.
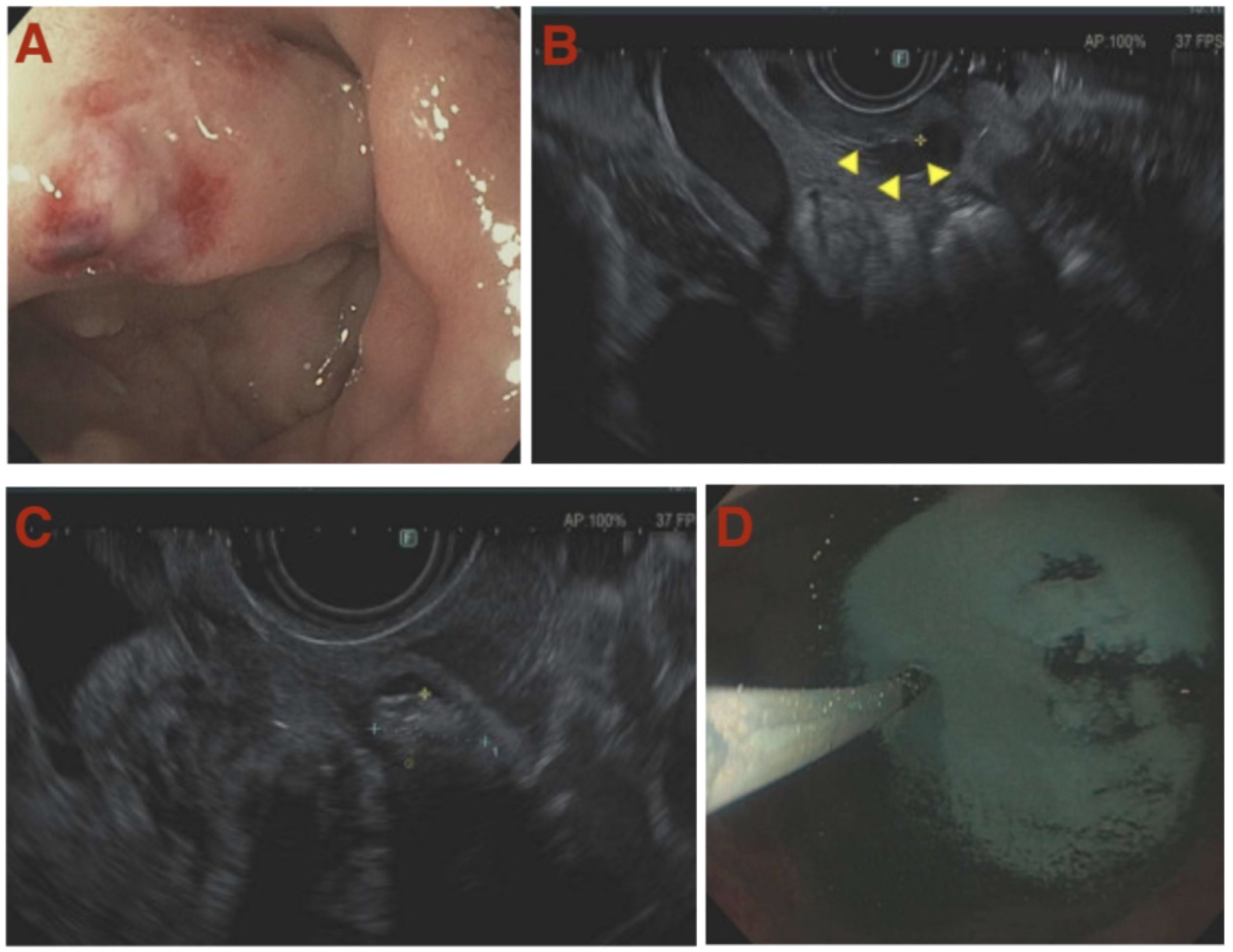
Figure: Figure 1: duodenal varix with whale sign (A), duodenal varix on EUS (B), cyanoacrylate injected (C), hemostatic powder deployment (D).
Disclosures:
Jessica Sosio indicated no relevant financial relationships.
Hani Shamseddeen indicated no relevant financial relationships.
Niharika Samala: Novo Nordisk – Consultant.
Umer Bhatti indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace Diagnostics – Consultant.
Jessica Sosio, DO1, Hani Shamseddeen, MD2, Niharika Samala, MD2, Umer Bhatti, MD2, Mohammad Al-Haddad, MD, FACG2. P1089 - Multi-Tool Endoscopic Management of Recalcitrant Bleeding Duodenal Varices in Portal, Splenic and Superior Mesenteric Vein Thromboses, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
