Sunday Poster Session
Category: Interventional Endoscopy
P1090 - The Unpredictable Migration of Biliary Stents
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- PA
Pranusha Atuluru, MD
University of Washington Medicine
Seattle, WA
Presenting Author(s)
Award: Presidential Poster Award
Pranusha Atuluru, MD, Yutaka Tomizawa, MD, MSc
University of Washington Medicine, Seattle, WA
Introduction: Endoscopic placement of plastic biliary stents is widely used as a modality of biliary decompression. Stent migration occurs unpredictably and has been reported in up to 6% of cases. There is limited data on timing and severity of adverse events caused by biliary stent migration. We report a rare case in which a migrated biliary stent caused fatal intestinal perforation even multiple years after placement.
Case Description/Methods: A 56-year-old man with history of colonic diverticulosis presented to an outside hospital with gallstone pancreatitis for which he underwent endoscopic retrograde cholangiopancreatography (ERCP) with plastic biliary stent placement followed by laparoscopic cholecystectomy. Patient underwent a repeat ERCP 3 months later with a plan for stent removal, but the stent was not found; therefore, it was assumed that patient had spontaneously passed the stent in stool.
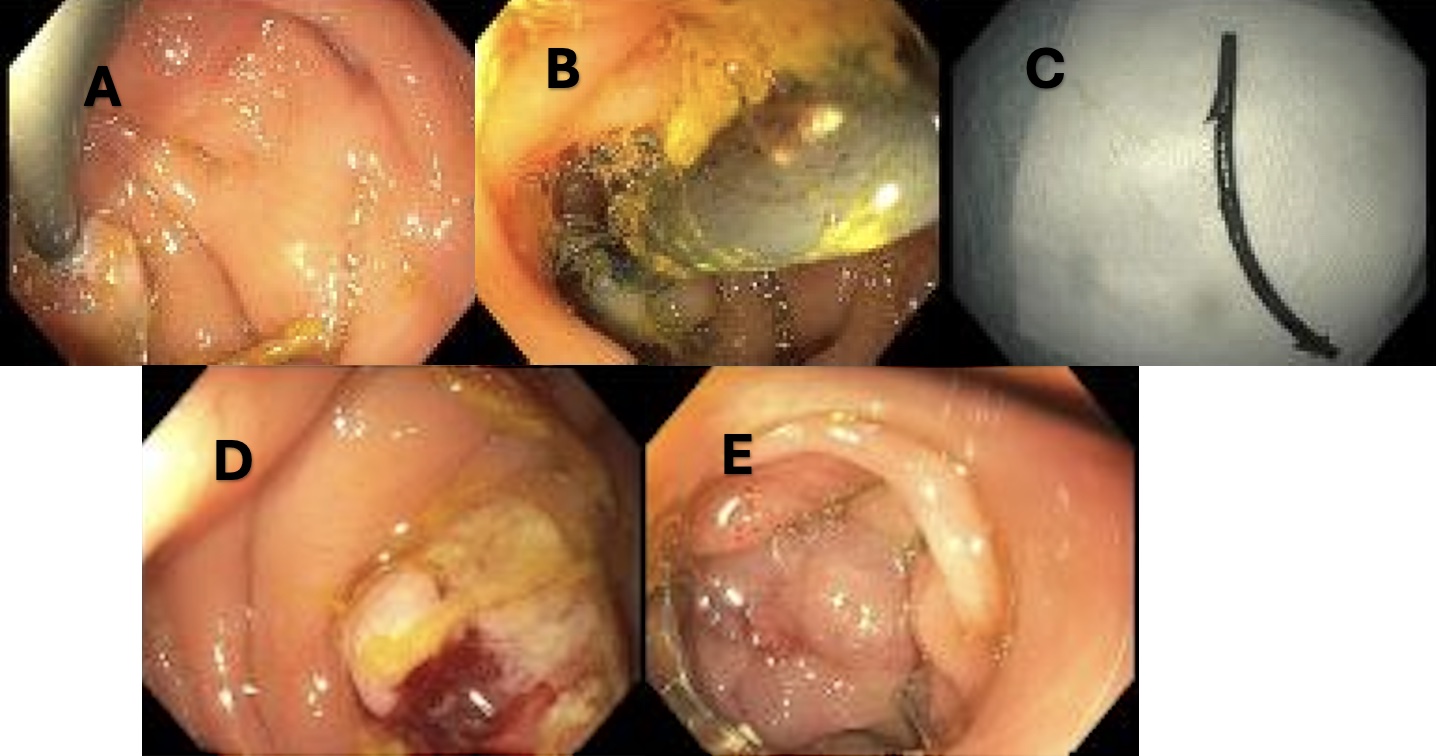
Two years later, the patient presented to our hospital with significant abdominal pain. CT showed a hallow intraluminal foreign body in the sigmoid colon with evidence of perforation and rim-enhancing fluid and gas collections adjacent to the foreign object. This raised initial concern for a retained biliary stent with colon perforation and abscesses (Fig 1a). Patient endorsed no other symptoms suggestive of peritonitis or sepsis. After multidisciplinary discussion with surgery, we decided to perform flexible sigmoidoscopy to remove the stent and endoscopically close the perforated site. A plastic biliary stent was found penetrating a sigmoid colon diverticulum (1b). The plastic stent was extracted (1c), a transmural defect was identified (1d) and closed by using an over-the-scope clip (1e). Patient tolerated procedure well and was discharged on oral antibiotics; he subsequently required further intervention for infection source control and ultimately fully recovered.
Discussion: It is noteworthy that our patient developed intestinal perforation from a migrated biliary stent multiple years after stent placement. To minimize complications, we propose that follow-up radiologic assessment with CT or X-ray should be more frequently considered when stent migration is suspected after a subsequent ERCP. Further, this case highlights that patients with certain predispositions such as diverticula or adhesions likely have increased perforation risk with stent migration; in such higher-risk cases endoscopic extraction followed by closure would be clinically warranted.
Disclosures:
Pranusha Atuluru, MD, Yutaka Tomizawa, MD, MSc. P1090 - The Unpredictable Migration of Biliary Stents, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Pranusha Atuluru, MD, Yutaka Tomizawa, MD, MSc
University of Washington Medicine, Seattle, WA
Introduction: Endoscopic placement of plastic biliary stents is widely used as a modality of biliary decompression. Stent migration occurs unpredictably and has been reported in up to 6% of cases. There is limited data on timing and severity of adverse events caused by biliary stent migration. We report a rare case in which a migrated biliary stent caused fatal intestinal perforation even multiple years after placement.
Case Description/Methods: A 56-year-old man with history of colonic diverticulosis presented to an outside hospital with gallstone pancreatitis for which he underwent endoscopic retrograde cholangiopancreatography (ERCP) with plastic biliary stent placement followed by laparoscopic cholecystectomy. Patient underwent a repeat ERCP 3 months later with a plan for stent removal, but the stent was not found; therefore, it was assumed that patient had spontaneously passed the stent in stool.
Two years later, the patient presented to our hospital with significant abdominal pain. CT showed a hallow intraluminal foreign body in the sigmoid colon with evidence of perforation and rim-enhancing fluid and gas collections adjacent to the foreign object. This raised initial concern for a retained biliary stent with colon perforation and abscesses (Fig 1a). Patient endorsed no other symptoms suggestive of peritonitis or sepsis. After multidisciplinary discussion with surgery, we decided to perform flexible sigmoidoscopy to remove the stent and endoscopically close the perforated site. A plastic biliary stent was found penetrating a sigmoid colon diverticulum (1b). The plastic stent was extracted (1c), a transmural defect was identified (1d) and closed by using an over-the-scope clip (1e). Patient tolerated procedure well and was discharged on oral antibiotics; he subsequently required further intervention for infection source control and ultimately fully recovered.
Discussion: It is noteworthy that our patient developed intestinal perforation from a migrated biliary stent multiple years after stent placement. To minimize complications, we propose that follow-up radiologic assessment with CT or X-ray should be more frequently considered when stent migration is suspected after a subsequent ERCP. Further, this case highlights that patients with certain predispositions such as diverticula or adhesions likely have increased perforation risk with stent migration; in such higher-risk cases endoscopic extraction followed by closure would be clinically warranted.
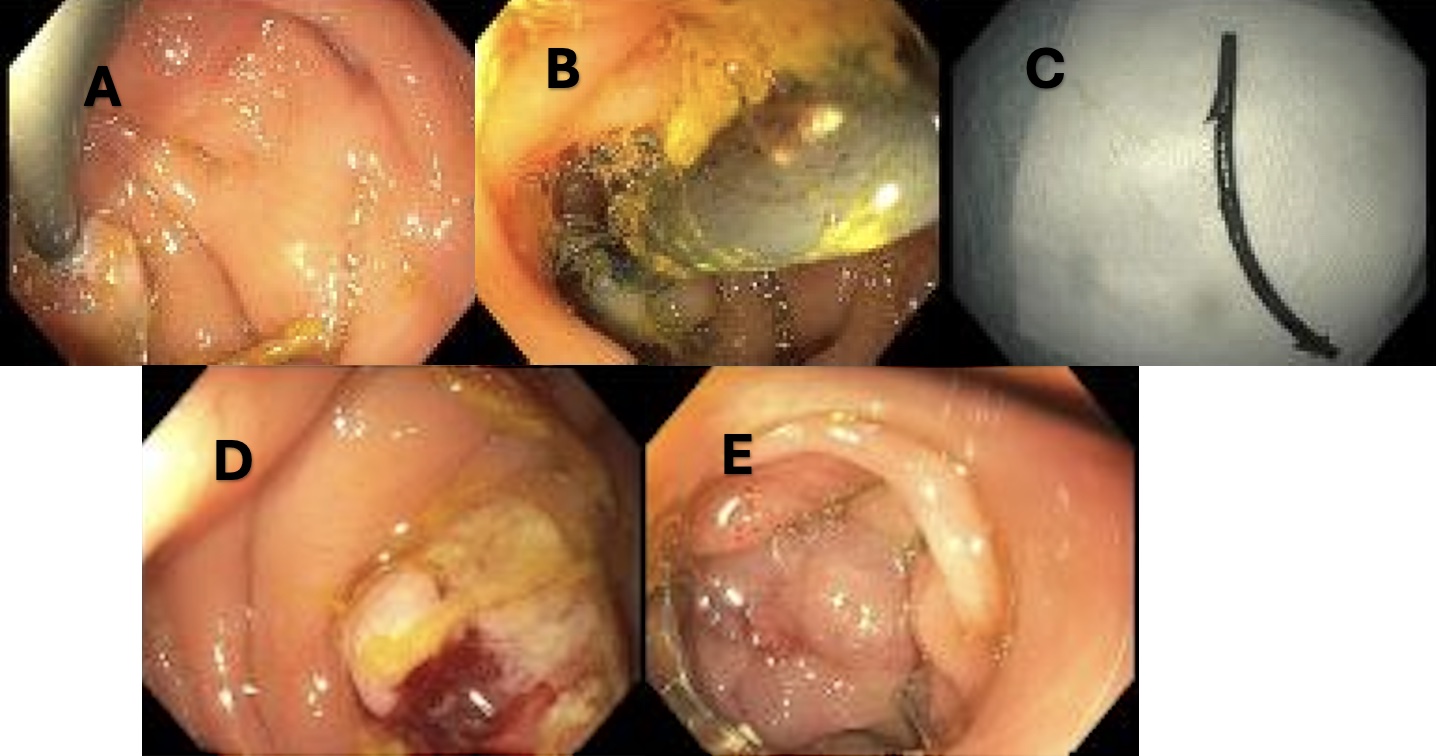
Figure: Figure 1: Endoscopic Pictures from Flexible Sigmoidoscopy. A) Stent penetrating through sigmoid colon. B) Stent Perforating Diverticulum. C) Plastic biliary stent after endoscopic removal. D) Site of perforation after stent removal. E) Perforation repaired with over-the-scope clip.
Disclosures:
Pranusha Atuluru indicated no relevant financial relationships.
Yutaka Tomizawa: AI Medical Service – Consultant. Boston Scientific – Consultant. Medtronic – Consultant.
Pranusha Atuluru, MD, Yutaka Tomizawa, MD, MSc. P1090 - The Unpredictable Migration of Biliary Stents, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

