Sunday Poster Session
Category: Interventional Endoscopy
P1094 - Cystic Duct Take Off From the Right Main Hepatic Duct: Case of an Interesting Anatomic Variant
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KO
Kashif Osmani, MD
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Kashif Osmani, MD1, Zeynep Ikiz, BS2, Grace Guzman, MD3, Cemal Yazici, MD1
1University of Illinois College of Medicine, Chicago, IL; 2Universidad Autónoma de Guadalajara, Chicago, IL; 3University of Illinois, Chicago, IL
Introduction: Understanding anatomic variations of the biliary tree is crucial for accurate diagnoses, effective endoscopic and surgical interventions, and prevention of potential complications like bile duct injury. Although advanced imaging modalities such as MRCP can help diagnose such anomalies, rare variants may be missed, and ERCP can play a crucial role in such scenarios.
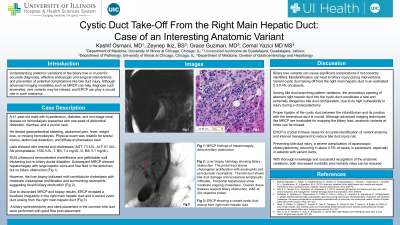
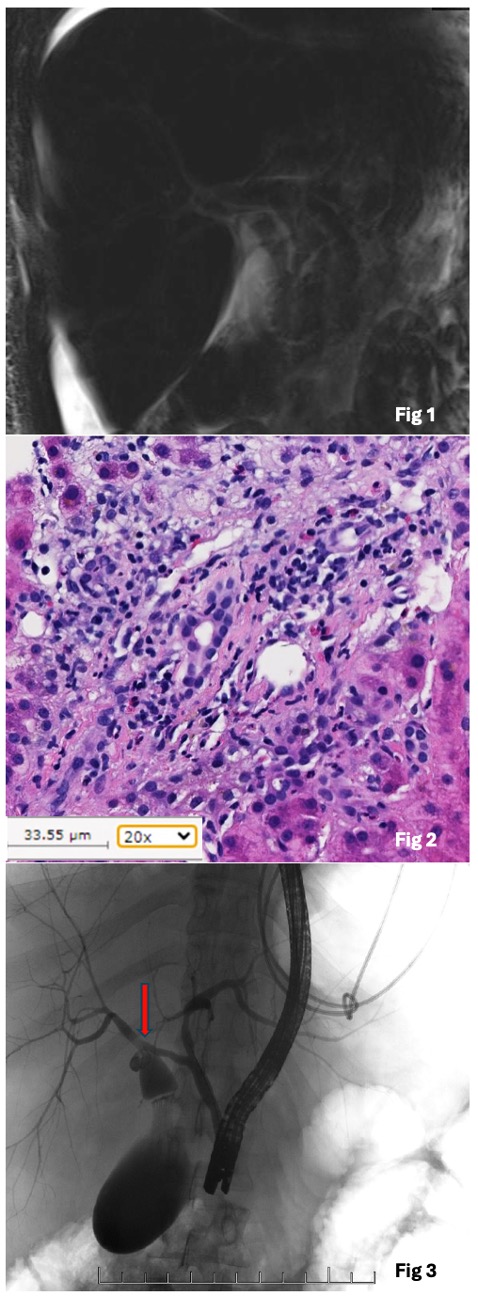
Case Description/Methods: A 41-year-old male with hypertension, diabetes, and end-stage renal disease on hemodialysis presented with one week of abdominal distention, diarrhea, and a pruritic rash. He denied gastrointestinal bleeding, abdominal pain, fever, weight loss, or missing hemodialysis. Physical exam was notable for scleral icterus, abdominal distention, and diffuse erythematous rash. Labs showed mild anemia and cholestasis (AST: 73 IU/L, ALT: 61 IU/L, Alk phosphatase: 1530 IU/L, T. Bili: 7.4 mg/dL, D. Bili: 5.1 mg/dL). RUQ ultrasound demonstrated cholelithiasis and gallbladder wall thickening but no biliary ductal dilatation. Subsequent MRCP showed hepatomegaly with large hepatic veins and free fluid in the abdomen but no biliary obstruction (Fig 1). However, the liver biopsy indicated mild centrilobular cholestasis with moderate cholangiolar proliferation and surrounding neutrophils, suggesting recent biliary obstruction (Fig 2). Due to discordant MRCP and biopsy results, ERCP revealed a localized irregularity in the right main hepatic duct and a variant cystic duct arising from the right main hepatic duct (Fig 3). A biliary sphincterotomy and stent placement in the common bile duct were performed with good flow post-placement.
Discussion: Biliary tree variants can cause significant complications if not correctly identified. Misidentification can lead to biliary injury during interventions. Variant cystic duct taking off from the right main hepatic duct in an estimated 0.3-0.4% of patients. Proper ligation of the cystic duct between the infundibulum and its junction with the anomalous duct is crucial. Although advanced imaging techniques like MRCP are invaluable for mapping the biliary tract, anatomic variants at times can be missed. ERCP is crucial in these cases for accurate identification of variant anatomy and interval management to reduce bile duct injury risk. Preventing bile duct injury, a severe complication of laparoscopic cholecystectomy, occurring in about 0.5% of cases, is paramount, especially in patients with variant ducts.
Disclosures:
Kashif Osmani, MD1, Zeynep Ikiz, BS2, Grace Guzman, MD3, Cemal Yazici, MD1. P1094 - Cystic Duct Take Off From the Right Main Hepatic Duct: Case of an Interesting Anatomic Variant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2Universidad Autónoma de Guadalajara, Chicago, IL; 3University of Illinois, Chicago, IL
Introduction: Understanding anatomic variations of the biliary tree is crucial for accurate diagnoses, effective endoscopic and surgical interventions, and prevention of potential complications like bile duct injury. Although advanced imaging modalities such as MRCP can help diagnose such anomalies, rare variants may be missed, and ERCP can play a crucial role in such scenarios.
Case Description/Methods: A 41-year-old male with hypertension, diabetes, and end-stage renal disease on hemodialysis presented with one week of abdominal distention, diarrhea, and a pruritic rash. He denied gastrointestinal bleeding, abdominal pain, fever, weight loss, or missing hemodialysis. Physical exam was notable for scleral icterus, abdominal distention, and diffuse erythematous rash. Labs showed mild anemia and cholestasis (AST: 73 IU/L, ALT: 61 IU/L, Alk phosphatase: 1530 IU/L, T. Bili: 7.4 mg/dL, D. Bili: 5.1 mg/dL). RUQ ultrasound demonstrated cholelithiasis and gallbladder wall thickening but no biliary ductal dilatation. Subsequent MRCP showed hepatomegaly with large hepatic veins and free fluid in the abdomen but no biliary obstruction (Fig 1). However, the liver biopsy indicated mild centrilobular cholestasis with moderate cholangiolar proliferation and surrounding neutrophils, suggesting recent biliary obstruction (Fig 2). Due to discordant MRCP and biopsy results, ERCP revealed a localized irregularity in the right main hepatic duct and a variant cystic duct arising from the right main hepatic duct (Fig 3). A biliary sphincterotomy and stent placement in the common bile duct were performed with good flow post-placement.
Discussion: Biliary tree variants can cause significant complications if not correctly identified. Misidentification can lead to biliary injury during interventions. Variant cystic duct taking off from the right main hepatic duct in an estimated 0.3-0.4% of patients. Proper ligation of the cystic duct between the infundibulum and its junction with the anomalous duct is crucial. Although advanced imaging techniques like MRCP are invaluable for mapping the biliary tract, anatomic variants at times can be missed. ERCP is crucial in these cases for accurate identification of variant anatomy and interval management to reduce bile duct injury risk. Preventing bile duct injury, a severe complication of laparoscopic cholecystectomy, occurring in about 0.5% of cases, is paramount, especially in patients with variant ducts.
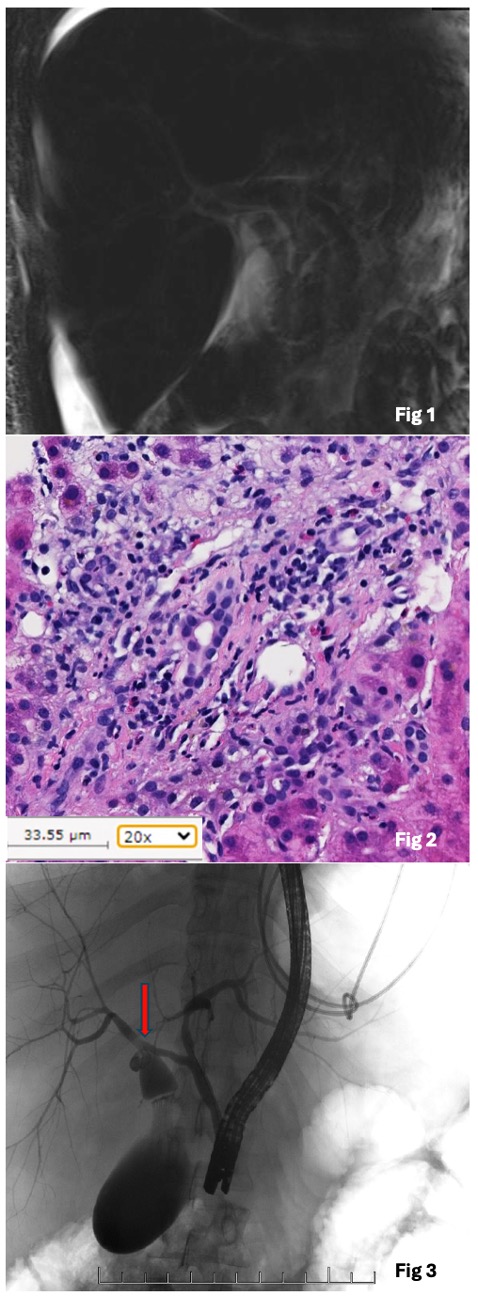
Figure: Fig 1: MRCP findings of hepatomegaly, without biliary obstruction.
Fig 2: Liver biopsy histology showing biliary obstruction. The portal tract shows cholangiolar proliferation with eosinophils and peri-ductular neutrophils. The bile duct shows bile duct damage and occasional lymphocytic infiltrates. Periportal hepatocytes show moderate ongoing cholestasis. Overall, these features support biliary obstruction.
Fig 3: ERCP showing a variant cystic duct arising from right main hepatic duct.
Fig 2: Liver biopsy histology showing biliary obstruction. The portal tract shows cholangiolar proliferation with eosinophils and peri-ductular neutrophils. The bile duct shows bile duct damage and occasional lymphocytic infiltrates. Periportal hepatocytes show moderate ongoing cholestasis. Overall, these features support biliary obstruction.
Fig 3: ERCP showing a variant cystic duct arising from right main hepatic duct.
Disclosures:
Kashif Osmani indicated no relevant financial relationships.
Zeynep Ikiz indicated no relevant financial relationships.
Grace Guzman indicated no relevant financial relationships.
Cemal Yazici indicated no relevant financial relationships.
Kashif Osmani, MD1, Zeynep Ikiz, BS2, Grace Guzman, MD3, Cemal Yazici, MD1. P1094 - Cystic Duct Take Off From the Right Main Hepatic Duct: Case of an Interesting Anatomic Variant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
