Sunday Poster Session
Category: Interventional Endoscopy
P1025 - Duodenal Stent Outcomes: A Retrospective Analysis of Clinical Success and Adverse Events in Patients With Malignant Gastric Outlet Obstructions
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

James Gore, DO
Ochsner Health Clinic Foundation
New Orleans, LA
Presenting Author(s)
James Gore, DO1, Ian Tobal, DO2, Wesley Villacencio-Torres, MD1, Janak Shah, MD1, Erin Biggs, PhD1, John Evans, MD1, Neej Patel, MD1, Ricardo Romero, MD1
1Ochsner Health Clinic Foundation, New Orleans, LA; 2Ochsner Medical Center, Jefferson, LA
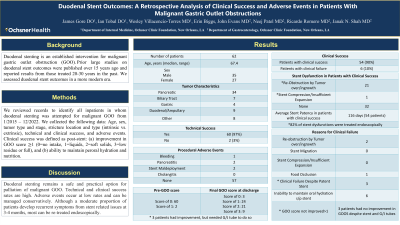
Introduction: Duodenal stenting is an established intervention for malignant gastric outlet obstruction (GOO). Prior large studies on duodenal stent outcomes were published over 15 years ago, and reported results from those treated 20-30 years in the past. We assessed duodenal stent outcomes in a more modern era.
Methods: We reviewed records to identify all inpatients in whom duodenal stenting was attempted for malignant GOO from 1/2015 – 12/2022. We collected the following data: Age, sex, tumor type and stage, stricture location and type (intrinsic vs. extrinsic), technical and clinical success, and adverse events. Clinical success was defined as post-stent: (a) improvement in GOO score ≥1 (0=no intake, 1=liquids, 2=soft solids, 3-low residue or full), and (b) ability to maintain peroral hydration and nutrition.
Results: Duodenal stenting was attempted in 62 patients (mean age 67 years, 56% male) over an 8-year period. Most had stage 4 disease (84%). Tumor types included pancreaticobiliary (66%), gastric/duodenal (21%), and other (13%). Most strictures were extrinsic (79%), and located at the 1st/2nd (64%) or 3rd/4th (24%) portions of the duodenum; or the pylorus (12%). Technical success was 97% (60/62). Procedural adverse events included bleeding (2%), treated with 1 unit transfusion; and two cases of mild pancreatitis (3%), treated with supportive care. Clinical success was seen in 90% (54/60). Clinical failures occurred due to short interval (< 48hrs) stent occlusion/insufficient expansion (n=2) and intolerability of oral intake despite successful stenting (n=4). Clinical failures were treated with venting gastrostomy tubes (n=2), feeding jejunostomy tubes (n=2), or both (n=2). Among patients with post stent clinical success, 22 (41%) developed recurrent GOO at median interval of 116 days due to: tissue ingrowth/overgrowth (n=21) or lumenal restenosis from tumor expansion (n=1). These patients were treated with repeat duodenal stenting (n=17), dilation (n=1), and surgical bypass (n=3). One patient with recurrent GOO opted for hospice care.
Discussion: Duodenal stenting remains a safe and practical option for palliation of malignant GOO. Technical and clinical success rates are high. Adverse events occur at low rates, and can be managed conservatively. Although a moderate proportion of patients develop recurrent symptoms from stent related issues at 3-4 months, most can be re-treated endoscopically.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
James Gore, DO1, Ian Tobal, DO2, Wesley Villacencio-Torres, MD1, Janak Shah, MD1, Erin Biggs, PhD1, John Evans, MD1, Neej Patel, MD1, Ricardo Romero, MD1. P1025 - Duodenal Stent Outcomes: A Retrospective Analysis of Clinical Success and Adverse Events in Patients With Malignant Gastric Outlet Obstructions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ochsner Health Clinic Foundation, New Orleans, LA; 2Ochsner Medical Center, Jefferson, LA
Introduction: Duodenal stenting is an established intervention for malignant gastric outlet obstruction (GOO). Prior large studies on duodenal stent outcomes were published over 15 years ago, and reported results from those treated 20-30 years in the past. We assessed duodenal stent outcomes in a more modern era.
Methods: We reviewed records to identify all inpatients in whom duodenal stenting was attempted for malignant GOO from 1/2015 – 12/2022. We collected the following data: Age, sex, tumor type and stage, stricture location and type (intrinsic vs. extrinsic), technical and clinical success, and adverse events. Clinical success was defined as post-stent: (a) improvement in GOO score ≥1 (0=no intake, 1=liquids, 2=soft solids, 3-low residue or full), and (b) ability to maintain peroral hydration and nutrition.
Results: Duodenal stenting was attempted in 62 patients (mean age 67 years, 56% male) over an 8-year period. Most had stage 4 disease (84%). Tumor types included pancreaticobiliary (66%), gastric/duodenal (21%), and other (13%). Most strictures were extrinsic (79%), and located at the 1st/2nd (64%) or 3rd/4th (24%) portions of the duodenum; or the pylorus (12%). Technical success was 97% (60/62). Procedural adverse events included bleeding (2%), treated with 1 unit transfusion; and two cases of mild pancreatitis (3%), treated with supportive care. Clinical success was seen in 90% (54/60). Clinical failures occurred due to short interval (< 48hrs) stent occlusion/insufficient expansion (n=2) and intolerability of oral intake despite successful stenting (n=4). Clinical failures were treated with venting gastrostomy tubes (n=2), feeding jejunostomy tubes (n=2), or both (n=2). Among patients with post stent clinical success, 22 (41%) developed recurrent GOO at median interval of 116 days due to: tissue ingrowth/overgrowth (n=21) or lumenal restenosis from tumor expansion (n=1). These patients were treated with repeat duodenal stenting (n=17), dilation (n=1), and surgical bypass (n=3). One patient with recurrent GOO opted for hospice care.
Discussion: Duodenal stenting remains a safe and practical option for palliation of malignant GOO. Technical and clinical success rates are high. Adverse events occur at low rates, and can be managed conservatively. Although a moderate proportion of patients develop recurrent symptoms from stent related issues at 3-4 months, most can be re-treated endoscopically.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
James Gore indicated no relevant financial relationships.
Ian Tobal indicated no relevant financial relationships.
Wesley Villacencio-Torres indicated no relevant financial relationships.
Janak Shah indicated no relevant financial relationships.
Erin Biggs indicated no relevant financial relationships.
John Evans indicated no relevant financial relationships.
Neej Patel indicated no relevant financial relationships.
Ricardo Romero indicated no relevant financial relationships.
James Gore, DO1, Ian Tobal, DO2, Wesley Villacencio-Torres, MD1, Janak Shah, MD1, Erin Biggs, PhD1, John Evans, MD1, Neej Patel, MD1, Ricardo Romero, MD1. P1025 - Duodenal Stent Outcomes: A Retrospective Analysis of Clinical Success and Adverse Events in Patients With Malignant Gastric Outlet Obstructions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
