Sunday Poster Session
Category: Interventional Endoscopy
P1028 - Pyloromyotomy/Pyloroplasty Versus Pyloric Electrical Stimulation and Botox (Botulinum Toxin) Injection for the Management of Gastroparesis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdul-Rahman F. Diab, MD
University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME
Ocala, FL
Presenting Author(s)
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Mehak Sachdeva, MD3, Kenneth Hackbarth, DO3, Alexander Thompson, MD3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Pyloromyotomy/pyloroplasty, pyloric electrical stimulation, and pyloric Botox (botulinum toxin) injection are interventions with well-established efficacy in the management of gastroparesis. However, it is unclear how these interventions compare to each other. We aimed to compare pyloromyotomy/pyloroplasty versus pyloric electrical stimulation and pyloric Botox (botulinum toxin) injection for the management of gastroparesis.
Methods: We conducted a systematic literature review following PRISMA guidelines to identify articles directly comparing pyloromyotomy/pyloroplasty versus pyloric electrical stimulation and Botox (botulinum toxin) injection for the management of gastroparesis. We utilized the random effects model and calculated odds ratios for dichotomous data as metrics for effect size.
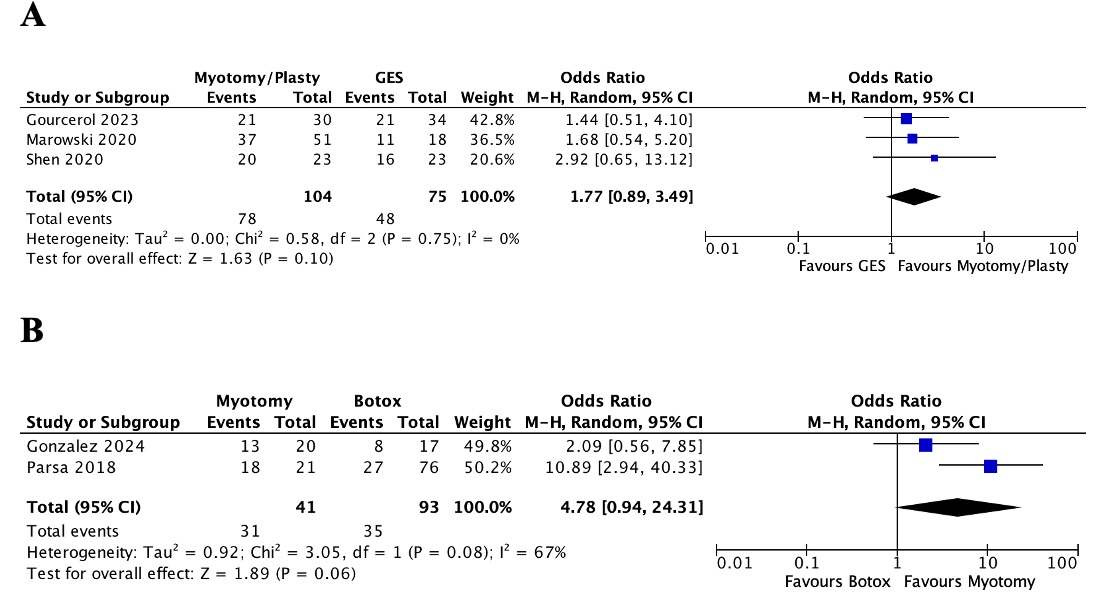
Results: Clinical success was reported in three studies comparing pyloromyotomy/pyloroplasty and pyloric electrical stimulation, involving 104 patients in the pyloromyotomy/pyloroplasty group and 75 patients in the pyloric electrical stimulation group. A statistically insignificant increase in clinical success was observed with pyloromyotomy/pyloroplasty compared to pyloric electrical stimulation (OR 1.77, 95% CI 0.89–3.49, p = 0.10, I² = 0%, p = 0.75). Clinical success was reported in two studies comparing pyloromyotomy and pyloric Botox (botulinum toxin) injection, involving 41 patients in the pyloromyotomy group and 93 patients in the pyloric Botox (botulinum toxin) injection group. A statistically insignificant increase in clinical success was observed with pyloromyotomy compared to pyloric Botox (botulinum toxin) injection (OR 4.78, 95% CI 0.94–24.31, p = 0.06, I² = 67%, p = 0.08).
Discussion: Although some evidence in the literature suggests superior efficacy of pyloromyotomy/pyloroplasty compared to pyloric electrical stimulation and Botox (botulinum toxin) injection for the management of gastroparesis, no pairwise meta-analysis level of evidence supports this to date. However, due to the consistent increase in clinical success observed with pyloromyotomy/pyloroplasty compared to pyloric electrical stimulation and Botox (botulinum toxin) injection across all studies in this meta-analysis, we believe that a larger pooled sample size (more studies) could support the superior efficacy of pyloromyotomy/pyloroplasty against pyloric electrical stimulation and Botox (botulinum toxin) injection for the management of gastroparesis.
Disclosures:
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Mehak Sachdeva, MD3, Kenneth Hackbarth, DO3, Alexander Thompson, MD3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P1028 - Pyloromyotomy/Pyloroplasty Versus Pyloric Electrical Stimulation and Botox (<i>Botulinum Toxin</i>) Injection for the Management of Gastroparesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Pyloromyotomy/pyloroplasty, pyloric electrical stimulation, and pyloric Botox (botulinum toxin) injection are interventions with well-established efficacy in the management of gastroparesis. However, it is unclear how these interventions compare to each other. We aimed to compare pyloromyotomy/pyloroplasty versus pyloric electrical stimulation and pyloric Botox (botulinum toxin) injection for the management of gastroparesis.
Methods: We conducted a systematic literature review following PRISMA guidelines to identify articles directly comparing pyloromyotomy/pyloroplasty versus pyloric electrical stimulation and Botox (botulinum toxin) injection for the management of gastroparesis. We utilized the random effects model and calculated odds ratios for dichotomous data as metrics for effect size.
Results: Clinical success was reported in three studies comparing pyloromyotomy/pyloroplasty and pyloric electrical stimulation, involving 104 patients in the pyloromyotomy/pyloroplasty group and 75 patients in the pyloric electrical stimulation group. A statistically insignificant increase in clinical success was observed with pyloromyotomy/pyloroplasty compared to pyloric electrical stimulation (OR 1.77, 95% CI 0.89–3.49, p = 0.10, I² = 0%, p = 0.75). Clinical success was reported in two studies comparing pyloromyotomy and pyloric Botox (botulinum toxin) injection, involving 41 patients in the pyloromyotomy group and 93 patients in the pyloric Botox (botulinum toxin) injection group. A statistically insignificant increase in clinical success was observed with pyloromyotomy compared to pyloric Botox (botulinum toxin) injection (OR 4.78, 95% CI 0.94–24.31, p = 0.06, I² = 67%, p = 0.08).
Discussion: Although some evidence in the literature suggests superior efficacy of pyloromyotomy/pyloroplasty compared to pyloric electrical stimulation and Botox (botulinum toxin) injection for the management of gastroparesis, no pairwise meta-analysis level of evidence supports this to date. However, due to the consistent increase in clinical success observed with pyloromyotomy/pyloroplasty compared to pyloric electrical stimulation and Botox (botulinum toxin) injection across all studies in this meta-analysis, we believe that a larger pooled sample size (more studies) could support the superior efficacy of pyloromyotomy/pyloroplasty against pyloric electrical stimulation and Botox (botulinum toxin) injection for the management of gastroparesis.
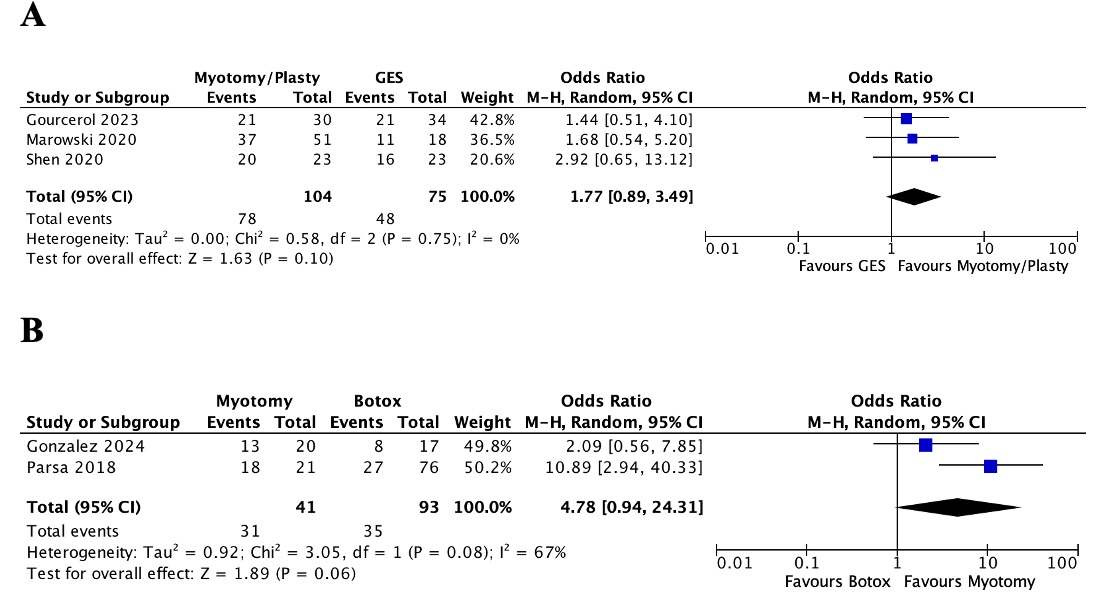
Figure: Forest plots comparing clinical success between pyloromyotomy/pyloroplasty and pyloric electrical stimulation (A), and between pyloromyotomy and pyloric Botox injection (B).
GES; gastric electrical stimulation.
GES; gastric electrical stimulation.
Disclosures:
Abdul-Rahman Diab indicated no relevant financial relationships.
Joseph Sujka indicated no relevant financial relationships.
Mehak Sachdeva indicated no relevant financial relationships.
Kenneth Hackbarth indicated no relevant financial relationships.
Alexander Thompson indicated no relevant financial relationships.
Salvatore Docimo indicated no relevant financial relationships.
Christopher DuCoin indicated no relevant financial relationships.
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Mehak Sachdeva, MD3, Kenneth Hackbarth, DO3, Alexander Thompson, MD3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P1028 - Pyloromyotomy/Pyloroplasty Versus Pyloric Electrical Stimulation and Botox (<i>Botulinum Toxin</i>) Injection for the Management of Gastroparesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
