Sunday Poster Session
Category: Interventional Endoscopy
P1033 - Endoscopic Submucosal Dissection (ESD) vs Transanal Endoscopic Microsurgery (TEM) for Resection of Early Epithelial and Subepithelial Rectal Tumors: A Meta-Analysis of 15 Studies
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdul-Rahman F. Diab, MD
University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME
Ocala, FL
Presenting Author(s)
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Mehak Sachdeva, MD3, Kenneth Hackbarth, DO3, Alexander Thompson, MD3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Early rectal tumors can be managed by Transanal Endoscopic Microsurgery (TEM) and Endoscopic Submucosal Dissection (ESD). This study aimed to compare ESD and TEM in the resection of early rectal tumors regarding en bloc resection, R0 resection, procedural time, perforations, bleeding, adverse events/complications, length of stay, cost from admission to discharge, and recurrence.
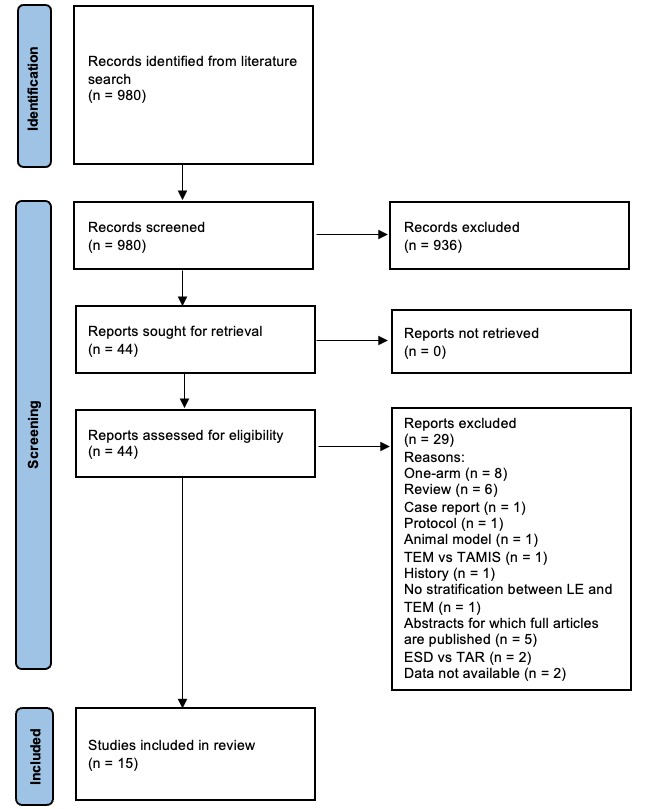
Methods: We conducted a systematic literature review following PRISMA guidelines to identify articles that directly compare ESD with TEM for the resection of rectal tumors. We utilized the random effects model and calculated odds ratios for dichotomous data, as well as mean differences for continuous data, to determine effect sizes. Subgroup analysis was performed based on tumor size differences between the two groups and whether the tumor was epithelial or subepithelial.
Results: The en bloc resection rate did not differ significantly between ESD and TEM overall, but subgroup analysis revealed a statistically significant increase in the en bloc resection rate with ESD compared to TEM in the epithelial subgroup. The R0 resection rate also did not differ overall, but subgroup analysis showed a statistically significant increase in R0 resection with ESD compared to TEM in the subepithelial subgroup, and in studies where there was no difference in tumor sizes. Procedural time was shorter in the ESD group, with a p-value of 0.05, exactly at the significance cutoff. There were no significant differences in perforation, bleeding, or total adverse events/complications between the groups. Length of stay was significantly shorter in the ESD group, and the cost from admission to discharge was lower with ESD. Recurrence rates were significantly lower in the ESD group. For a detailed and quantitative description of the results, please refer to the accompanying table.
Discussion: This study suggests the superiority of ESD over TEM in several aspects. However, a major limitation of this meta-analysis is that only 2 out of the 15 included studies used propensity matching of patients between the ESD and TEM groups. Randomized controlled trials or at least prospective propensity-matched studies are needed to reassess our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Mehak Sachdeva, MD3, Kenneth Hackbarth, DO3, Alexander Thompson, MD3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P1033 - Endoscopic Submucosal Dissection (ESD) vs Transanal Endoscopic Microsurgery (TEM) for Resection of Early Epithelial and Subepithelial Rectal Tumors: A Meta-Analysis of 15 Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Early rectal tumors can be managed by Transanal Endoscopic Microsurgery (TEM) and Endoscopic Submucosal Dissection (ESD). This study aimed to compare ESD and TEM in the resection of early rectal tumors regarding en bloc resection, R0 resection, procedural time, perforations, bleeding, adverse events/complications, length of stay, cost from admission to discharge, and recurrence.
Methods: We conducted a systematic literature review following PRISMA guidelines to identify articles that directly compare ESD with TEM for the resection of rectal tumors. We utilized the random effects model and calculated odds ratios for dichotomous data, as well as mean differences for continuous data, to determine effect sizes. Subgroup analysis was performed based on tumor size differences between the two groups and whether the tumor was epithelial or subepithelial.
Results: The en bloc resection rate did not differ significantly between ESD and TEM overall, but subgroup analysis revealed a statistically significant increase in the en bloc resection rate with ESD compared to TEM in the epithelial subgroup. The R0 resection rate also did not differ overall, but subgroup analysis showed a statistically significant increase in R0 resection with ESD compared to TEM in the subepithelial subgroup, and in studies where there was no difference in tumor sizes. Procedural time was shorter in the ESD group, with a p-value of 0.05, exactly at the significance cutoff. There were no significant differences in perforation, bleeding, or total adverse events/complications between the groups. Length of stay was significantly shorter in the ESD group, and the cost from admission to discharge was lower with ESD. Recurrence rates were significantly lower in the ESD group. For a detailed and quantitative description of the results, please refer to the accompanying table.
Discussion: This study suggests the superiority of ESD over TEM in several aspects. However, a major limitation of this meta-analysis is that only 2 out of the 15 included studies used propensity matching of patients between the ESD and TEM groups. Randomized controlled trials or at least prospective propensity-matched studies are needed to reassess our findings.
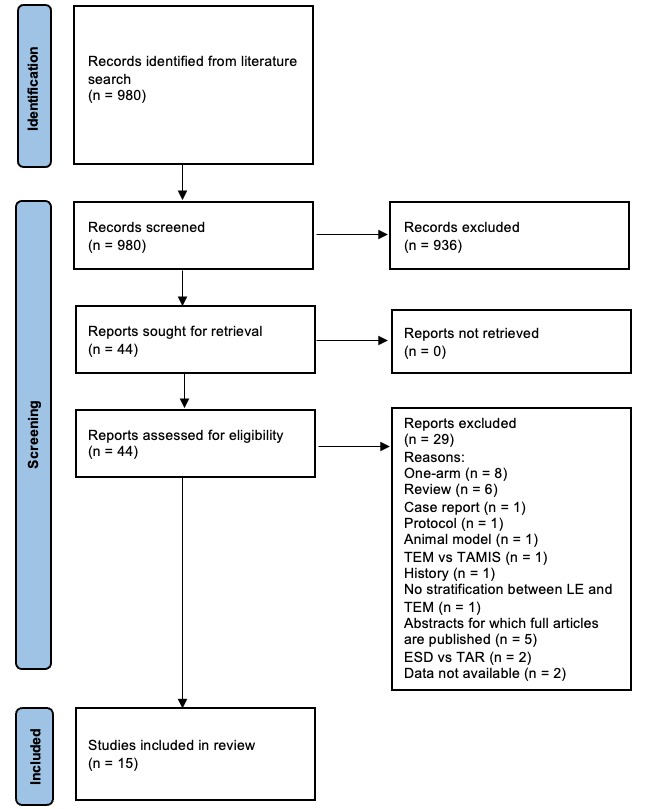
Figure: Literature Review Flow Diagram According to the PRISMA Guidelines
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdul-Rahman Diab indicated no relevant financial relationships.
Joseph Sujka indicated no relevant financial relationships.
Mehak Sachdeva indicated no relevant financial relationships.
Kenneth Hackbarth indicated no relevant financial relationships.
Alexander Thompson indicated no relevant financial relationships.
Salvatore Docimo indicated no relevant financial relationships.
Christopher DuCoin indicated no relevant financial relationships.
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Mehak Sachdeva, MD3, Kenneth Hackbarth, DO3, Alexander Thompson, MD3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P1033 - Endoscopic Submucosal Dissection (ESD) vs Transanal Endoscopic Microsurgery (TEM) for Resection of Early Epithelial and Subepithelial Rectal Tumors: A Meta-Analysis of 15 Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
