Sunday Poster Session
Category: Interventional Endoscopy
P1037 - Comparative Outcomes of Flexible Endoscopic Repair versus Surgical Repair in Zenker’s Diverticulum: A Matched Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Akua Nuako, MD
Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Akua Nuako, MD1, Steven Steinway, MD, PhD2, Bianca Zussino, 1, Erik Almazan, MD2, Nathon Smith, BS2, Kimberly Schuster, BS2, Alexandra Goad, BS1, Michele Ryan, MS2, Christopher C.. Thompson, MD, MSc3
1Massachusetts General Hospital, Boston, MA; 2Brigham and Women's Hospital, Boston, MA; 3Brigham and Women's Hospital, Harvard Medical School, Boston, MA
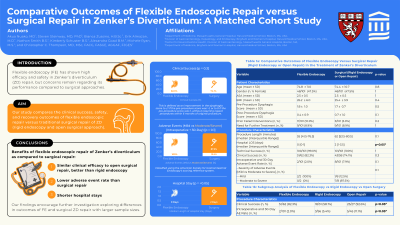
Introduction: Existing studies on endoscopic Zenker’s diverticulum (ZD) repair show high efficacy and safety. However, concerns remain regarding efficacy and safety compared to surgical approaches. We conducted a retrospective matched cohort study comparing the clinical efficacy and adverse events (AEs) between flexible endoscopic (FE) and surgical (rigid endoscopy and open technique) repair of ZD.
Methods: We included 198 patients who underwent ZD repair (FE: n=99, surgery: n=99) who were matched for age, gender, and ASA score. Clinical success was defined as an improvement in the dysphagia score to ≤1 if the pre-procedure score was >1 or to 0 if the pre-procedure score was 1, without the need for repeat procedures within >6 months. Secondary outcomes included technical success (completion of all intended procedure steps), AE rates, procedure length, hospital length of stay (LOS), and need for further treatment. AEs were classified using the American Society for Gastrointestinal Endoscopy’s scoring reference system.
Results: Baseline characteristics were similar between the FE and surgical cohort (Table 1). There was a trend towards higher clinical success in the FE cohort compared to the surgical cohort (82.0% vs. 74.1%, respectively), though this difference was not statistically significant (p=0.42).
The AE rate was 3.03% (FE) vs 9.09% (surgery); however, this difference was not statistically significant (p = 0.13). The FE cohort did not have moderate or severe AEs, in contrast to the surgical cohort. Technical success was achieved in all cases with similar median procedure length time, need for further treatment, and median follow-up time between the FE and surgical cohorts. The FE group had a lower median hospital LOS (0 vs. 2 days) (p< 0.0001).
Discussion: In addition to similar clinical efficacy, flexible endoscopic repair of Zenker’s diverticulum demonstrated a lower combined intra-operative and 30-day AE rate compared to surgical repair, although this difference was not statistically significant. Notably, the AEs in the FE group were exclusively mild, contrasting with the varied severity of events in the surgical group. In addition to its safety profile, FE repair offers the advantage of shorter hospital stays compared to surgical repair. Our findings encourage further investigation exploring differences in outcomes of FE and surgical ZD repair with larger sample sizes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Akua Nuako, MD1, Steven Steinway, MD, PhD2, Bianca Zussino, 1, Erik Almazan, MD2, Nathon Smith, BS2, Kimberly Schuster, BS2, Alexandra Goad, BS1, Michele Ryan, MS2, Christopher C.. Thompson, MD, MSc3. P1037 - Comparative Outcomes of Flexible Endoscopic Repair versus Surgical Repair in Zenker’s Diverticulum: A Matched Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Massachusetts General Hospital, Boston, MA; 2Brigham and Women's Hospital, Boston, MA; 3Brigham and Women's Hospital, Harvard Medical School, Boston, MA
Introduction: Existing studies on endoscopic Zenker’s diverticulum (ZD) repair show high efficacy and safety. However, concerns remain regarding efficacy and safety compared to surgical approaches. We conducted a retrospective matched cohort study comparing the clinical efficacy and adverse events (AEs) between flexible endoscopic (FE) and surgical (rigid endoscopy and open technique) repair of ZD.
Methods: We included 198 patients who underwent ZD repair (FE: n=99, surgery: n=99) who were matched for age, gender, and ASA score. Clinical success was defined as an improvement in the dysphagia score to ≤1 if the pre-procedure score was >1 or to 0 if the pre-procedure score was 1, without the need for repeat procedures within >6 months. Secondary outcomes included technical success (completion of all intended procedure steps), AE rates, procedure length, hospital length of stay (LOS), and need for further treatment. AEs were classified using the American Society for Gastrointestinal Endoscopy’s scoring reference system.
Results: Baseline characteristics were similar between the FE and surgical cohort (Table 1). There was a trend towards higher clinical success in the FE cohort compared to the surgical cohort (82.0% vs. 74.1%, respectively), though this difference was not statistically significant (p=0.42).
The AE rate was 3.03% (FE) vs 9.09% (surgery); however, this difference was not statistically significant (p = 0.13). The FE cohort did not have moderate or severe AEs, in contrast to the surgical cohort. Technical success was achieved in all cases with similar median procedure length time, need for further treatment, and median follow-up time between the FE and surgical cohorts. The FE group had a lower median hospital LOS (0 vs. 2 days) (p< 0.0001).
Discussion: In addition to similar clinical efficacy, flexible endoscopic repair of Zenker’s diverticulum demonstrated a lower combined intra-operative and 30-day AE rate compared to surgical repair, although this difference was not statistically significant. Notably, the AEs in the FE group were exclusively mild, contrasting with the varied severity of events in the surgical group. In addition to its safety profile, FE repair offers the advantage of shorter hospital stays compared to surgical repair. Our findings encourage further investigation exploring differences in outcomes of FE and surgical ZD repair with larger sample sizes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Akua Nuako indicated no relevant financial relationships.
Steven Steinway indicated no relevant financial relationships.
Bianca Zussino indicated no relevant financial relationships.
Erik Almazan indicated no relevant financial relationships.
Nathon Smith indicated no relevant financial relationships.
Kimberly Schuster indicated no relevant financial relationships.
Alexandra Goad indicated no relevant financial relationships.
Michele Ryan indicated no relevant financial relationships.
Christopher Thompson: Apollo Endosurgery – Consultant, Grant/Research Support. Bariendo – Consultant, Founder, Owner/Ownership Interest. Boston Scientific – Consultant, Grant/Research Support. Endoquest Robotics – Advisory Committee/Board Member, Consultant, Grant/Research Support. Endosim – Royalties. Enterasense Ltd. – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Stock Options. EnVision Endoscopy – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Stock Options. ERBE – Grant/Research Support. Fractyl – Consultant, Grant/Research Support, Stock Options. Fujifilm – Grant/Research Support. GI Dynamics – Consultant, Grant/Research Support. GI Windows – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Royalties, Stock Options. Lumendi – Grant/Research Support. Medtronic – Advisory Committee/Board Member, Consultant. Olympus – Consultant, Grant/Research Support. USGI Medical – Advisory Committee/Board Member, Consultant, Grant/Research Support. Xenter – Advisory Committee/Board Member, Consultant.
Akua Nuako, MD1, Steven Steinway, MD, PhD2, Bianca Zussino, 1, Erik Almazan, MD2, Nathon Smith, BS2, Kimberly Schuster, BS2, Alexandra Goad, BS1, Michele Ryan, MS2, Christopher C.. Thompson, MD, MSc3. P1037 - Comparative Outcomes of Flexible Endoscopic Repair versus Surgical Repair in Zenker’s Diverticulum: A Matched Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
