Sunday Poster Session
Category: Interventional Endoscopy
P1040 - Accuracy of Intra-Operative Cholangiogram for Detection of Choledocholithiasis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- DK
Do Han Kim, MD
Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Award: Presidential Poster Award
Do Han Kim, MD1, Allison A. Marshall, MD, MPH2, Yousaf Hadi, MD3, Haley Waite, MS4, Jacquelin Florio, PA-C2, Nikhil Kumta, MD, MS2, Satish Nagula, MD2, Nicholas Hoerter, MD2
1Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai Hospital, New York, NY; 4Mount Sinai Health System, New York, NY
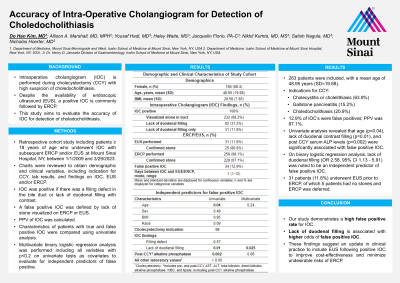
Introduction: Intraoperative cholangiogram (IOC) is performed during cholecystectomy (CCY) with high suspicion of choledocholithiasis. Despite the availability of endoscopic ultrasound (EUS), a positive IOC is commonly followed by endoscopic retrograde cholangiopancreatography (ERCP). This study aims to evaluate the accuracy of IOC for detection of choledocholithiasis.
Methods: We conducted a retrospective cohort study including patients ≥ 18 years of age who underwent IOC with subsequent ERCP and/or EUS at Mount Sinai Hospital, New York, between 1/1/2009 and 3/29/2023. Charts were reviewed to obtain demographic and clinical variables, including indication for CCY, lab results, and findings on IOC, EUS and/or ERCP. The IOC was positive if there was a filling defect in the bile duct or lack of duodenal filling with contrast. A false positive IOC was defined by lack of stone visualized on ERCP or EUS. Positive predictive value (PPV) of IOC was calculated; characteristics of patients with true and false positive IOC were compared using univariate analysis; multivariate binary logistic regression analysis was performed including all variables with p < 0.2 on univariate tests as covariates to evaluate for independent predictors of false positive.
Results: 263 patients were included, with a mean age of 48.95 years (SD=19.68). Indications for CCY were cholecystitis or cholelithiasis (63.9%), gallstone pancreatitis (15.2%) and choledocholithiasis (20.9%) (Table 1). Mean time from IOC to ERCP and/or EUS was 1 day (SD= 1.2). 12.9% of IOC’s were false positives; PPV was 87.1%.
Univariate analysis revealed that age (p=0.04), lack of duodenal contrast filling (p=0.01), and post CCY serum alkaline phosphatase levels (p=0.002) were significantly associated with false positive IOC. On binary logistic regression analysis, lack of duodenal filling (OR 2.58, 95% CI 1.13 - 5.91) was noted to be an independent predictor of false positive IOC.
31 patients (11.8%) underwent EUS prior to ERCP, of which 5 patients had no stones and ERCP was deferred. None of the patients in the cohort developed choledocholithiasis, cholangitis or pancreatitis at follow up (mean 13.3 months).
Discussion: Our study demonstrates a high false positive rate for IOC. Lack of duodenal filling is associated with higher odds of false positive IOC. These findings suggest an update in clinical practice to include EUS following positive IOC to improve cost-effectiveness and minimize undesirable risks of ERCP.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Do Han Kim, MD1, Allison A. Marshall, MD, MPH2, Yousaf Hadi, MD3, Haley Waite, MS4, Jacquelin Florio, PA-C2, Nikhil Kumta, MD, MS2, Satish Nagula, MD2, Nicholas Hoerter, MD2. P1040 - Accuracy of Intra-Operative Cholangiogram for Detection of Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Do Han Kim, MD1, Allison A. Marshall, MD, MPH2, Yousaf Hadi, MD3, Haley Waite, MS4, Jacquelin Florio, PA-C2, Nikhil Kumta, MD, MS2, Satish Nagula, MD2, Nicholas Hoerter, MD2
1Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai Hospital, New York, NY; 4Mount Sinai Health System, New York, NY
Introduction: Intraoperative cholangiogram (IOC) is performed during cholecystectomy (CCY) with high suspicion of choledocholithiasis. Despite the availability of endoscopic ultrasound (EUS), a positive IOC is commonly followed by endoscopic retrograde cholangiopancreatography (ERCP). This study aims to evaluate the accuracy of IOC for detection of choledocholithiasis.
Methods: We conducted a retrospective cohort study including patients ≥ 18 years of age who underwent IOC with subsequent ERCP and/or EUS at Mount Sinai Hospital, New York, between 1/1/2009 and 3/29/2023. Charts were reviewed to obtain demographic and clinical variables, including indication for CCY, lab results, and findings on IOC, EUS and/or ERCP. The IOC was positive if there was a filling defect in the bile duct or lack of duodenal filling with contrast. A false positive IOC was defined by lack of stone visualized on ERCP or EUS. Positive predictive value (PPV) of IOC was calculated; characteristics of patients with true and false positive IOC were compared using univariate analysis; multivariate binary logistic regression analysis was performed including all variables with p < 0.2 on univariate tests as covariates to evaluate for independent predictors of false positive.
Results: 263 patients were included, with a mean age of 48.95 years (SD=19.68). Indications for CCY were cholecystitis or cholelithiasis (63.9%), gallstone pancreatitis (15.2%) and choledocholithiasis (20.9%) (Table 1). Mean time from IOC to ERCP and/or EUS was 1 day (SD= 1.2). 12.9% of IOC’s were false positives; PPV was 87.1%.
Univariate analysis revealed that age (p=0.04), lack of duodenal contrast filling (p=0.01), and post CCY serum alkaline phosphatase levels (p=0.002) were significantly associated with false positive IOC. On binary logistic regression analysis, lack of duodenal filling (OR 2.58, 95% CI 1.13 - 5.91) was noted to be an independent predictor of false positive IOC.
31 patients (11.8%) underwent EUS prior to ERCP, of which 5 patients had no stones and ERCP was deferred. None of the patients in the cohort developed choledocholithiasis, cholangitis or pancreatitis at follow up (mean 13.3 months).
Discussion: Our study demonstrates a high false positive rate for IOC. Lack of duodenal filling is associated with higher odds of false positive IOC. These findings suggest an update in clinical practice to include EUS following positive IOC to improve cost-effectiveness and minimize undesirable risks of ERCP.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Do Han Kim indicated no relevant financial relationships.
Allison Marshall indicated no relevant financial relationships.
Yousaf Hadi indicated no relevant financial relationships.
Haley Waite indicated no relevant financial relationships.
Jacquelin Florio indicated no relevant financial relationships.
Nikhil Kumta: Apollo – Consultant, Speakers Bureau. Boston Scientific – Consultant, Speakers Bureau. Olympus – Consultant.
Satish Nagula indicated no relevant financial relationships.
Nicholas Hoerter: Redesign Health – Stock-privately held company.
Do Han Kim, MD1, Allison A. Marshall, MD, MPH2, Yousaf Hadi, MD3, Haley Waite, MS4, Jacquelin Florio, PA-C2, Nikhil Kumta, MD, MS2, Satish Nagula, MD2, Nicholas Hoerter, MD2. P1040 - Accuracy of Intra-Operative Cholangiogram for Detection of Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

