Sunday Poster Session
Category: IBD
P0953 - Racial Differences in the Use of and Suboptimal Clinical Responses to Anti-TNF Therapy for Patients with Inflammatory Bowel Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Jennifer Youn, MD
Tufts Medical Center
Boston, MA
Presenting Author(s)
Jennifer Youn, MD1, Ye Chen, MSc1, Sonia Friedman, MD2
1Tufts Medical Center, Boston, MA; 2Tufts University School of Medicine, Boston, MA
Introduction: The prevalence of inflammatory bowel disease (IBD) in non-White populations is rapidly increasing globally. This study aims to compare the racial differences in the use of and suboptimal clinical responses to anti-tumor necrosis factor (TNF) therapy for patients with IBD.
Methods: We conducted a retrospective cohort study of adult IBD patients treated at a tertiary care center from 2010 to 2023. All patients with IBD and self-identifying as White, Black, or Asian were included. Patients who received anti-TNF therapy were observed for 1 year after the initiation. Suboptimal clinical responses to anti-TNF therapy were measured by addition of 5-amiosalicylate (ASA), addition of steroid, addition of immunomodulator, switch in biologics, IBD-related hospitalizations, and/or IBD-related surgeries. For statistical analysis, Chi-square tests were used to compare patient demographics and medication use. For analysis of suboptimal clinical responses, multivariable logistic regression models were applied and adjusted for confounders (age, sex, duration of disease) to compute adjusted odds radios (aOR) with 95% confidence interval (95%CI).
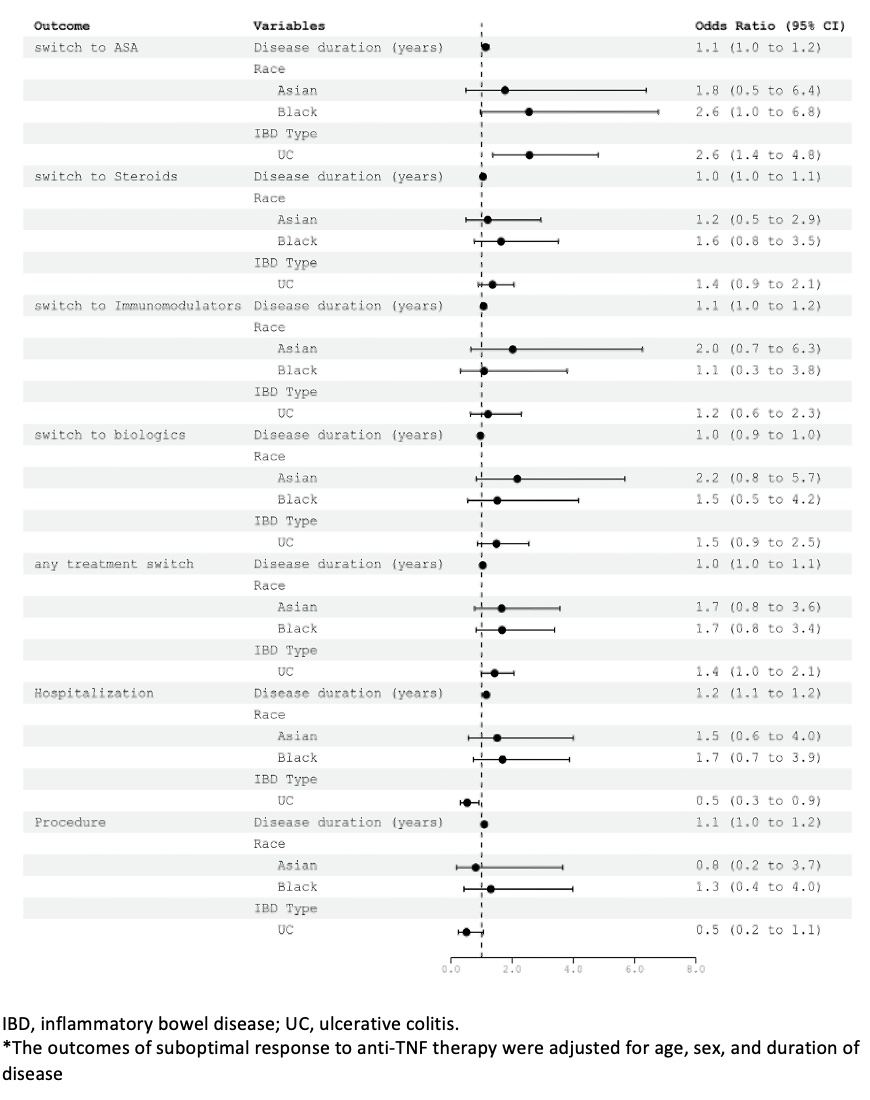
Results: A total of 2715 IBD patients were identified. Asian patients were less likely to receive anti-TNF agents compared to Black and White patients (p=0.027). Black patients were more likely to receive steroid medications at least once compared to Asian and White patients (p=0.046). A total of 605 patients received anti-TNF therapy; which 540(89.3%) were White, 30(5.9%) were Asians, and 35(5.8%) were Black. After multivariable regression, there were no statistical differences in suboptimal responses to anti-TNF therapy between Asian and Black patients compared to White patients: addition of ASA(Asian aOR1.8 [95%CI 0.5-6.4]; Black aOR2.6 [95%CI 1.0-6.8]), addition of steroid(Asian aOR1.2 [95%CI 0.5-2.9]; Black aOR1.6 [95%CI 0.8-3.5]), addition of immunomodulator(Asian aOR2.0 [95%CI 0.7-6.3]; Black aOR1.1 [95%CI 0.3-3.8]), switch in biologics(Asian aOR2.2 [95%CI 0.8-5.7]; Black aOR1.5 [95%CI 0.5-4.2]), IBD-related hospitalizations(Asian aOR1.5 [95%CI 0.6-4.0]; Black aOR1.7 [95%CI 0.7-3.9]), and IBD-related surgeries(Asian aOR0.8 [95%CI 0.2-3.7]; Black aOR1.3 [95%CI 0.4-4.9]).
Discussion: Asian patients were less likely to receive anti-TNF therapy. There were no significant differences in suboptimal clinical responses to anti-TNF therapy between races. There is a need for further research in diverse racial groups to provide inclusive care to the IBD community.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jennifer Youn, MD1, Ye Chen, MSc1, Sonia Friedman, MD2. P0953 - Racial Differences in the Use of and Suboptimal Clinical Responses to Anti-TNF Therapy for Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2Tufts University School of Medicine, Boston, MA
Introduction: The prevalence of inflammatory bowel disease (IBD) in non-White populations is rapidly increasing globally. This study aims to compare the racial differences in the use of and suboptimal clinical responses to anti-tumor necrosis factor (TNF) therapy for patients with IBD.
Methods: We conducted a retrospective cohort study of adult IBD patients treated at a tertiary care center from 2010 to 2023. All patients with IBD and self-identifying as White, Black, or Asian were included. Patients who received anti-TNF therapy were observed for 1 year after the initiation. Suboptimal clinical responses to anti-TNF therapy were measured by addition of 5-amiosalicylate (ASA), addition of steroid, addition of immunomodulator, switch in biologics, IBD-related hospitalizations, and/or IBD-related surgeries. For statistical analysis, Chi-square tests were used to compare patient demographics and medication use. For analysis of suboptimal clinical responses, multivariable logistic regression models were applied and adjusted for confounders (age, sex, duration of disease) to compute adjusted odds radios (aOR) with 95% confidence interval (95%CI).
Results: A total of 2715 IBD patients were identified. Asian patients were less likely to receive anti-TNF agents compared to Black and White patients (p=0.027). Black patients were more likely to receive steroid medications at least once compared to Asian and White patients (p=0.046). A total of 605 patients received anti-TNF therapy; which 540(89.3%) were White, 30(5.9%) were Asians, and 35(5.8%) were Black. After multivariable regression, there were no statistical differences in suboptimal responses to anti-TNF therapy between Asian and Black patients compared to White patients: addition of ASA(Asian aOR1.8 [95%CI 0.5-6.4]; Black aOR2.6 [95%CI 1.0-6.8]), addition of steroid(Asian aOR1.2 [95%CI 0.5-2.9]; Black aOR1.6 [95%CI 0.8-3.5]), addition of immunomodulator(Asian aOR2.0 [95%CI 0.7-6.3]; Black aOR1.1 [95%CI 0.3-3.8]), switch in biologics(Asian aOR2.2 [95%CI 0.8-5.7]; Black aOR1.5 [95%CI 0.5-4.2]), IBD-related hospitalizations(Asian aOR1.5 [95%CI 0.6-4.0]; Black aOR1.7 [95%CI 0.7-3.9]), and IBD-related surgeries(Asian aOR0.8 [95%CI 0.2-3.7]; Black aOR1.3 [95%CI 0.4-4.9]).
Discussion: Asian patients were less likely to receive anti-TNF therapy. There were no significant differences in suboptimal clinical responses to anti-TNF therapy between races. There is a need for further research in diverse racial groups to provide inclusive care to the IBD community.
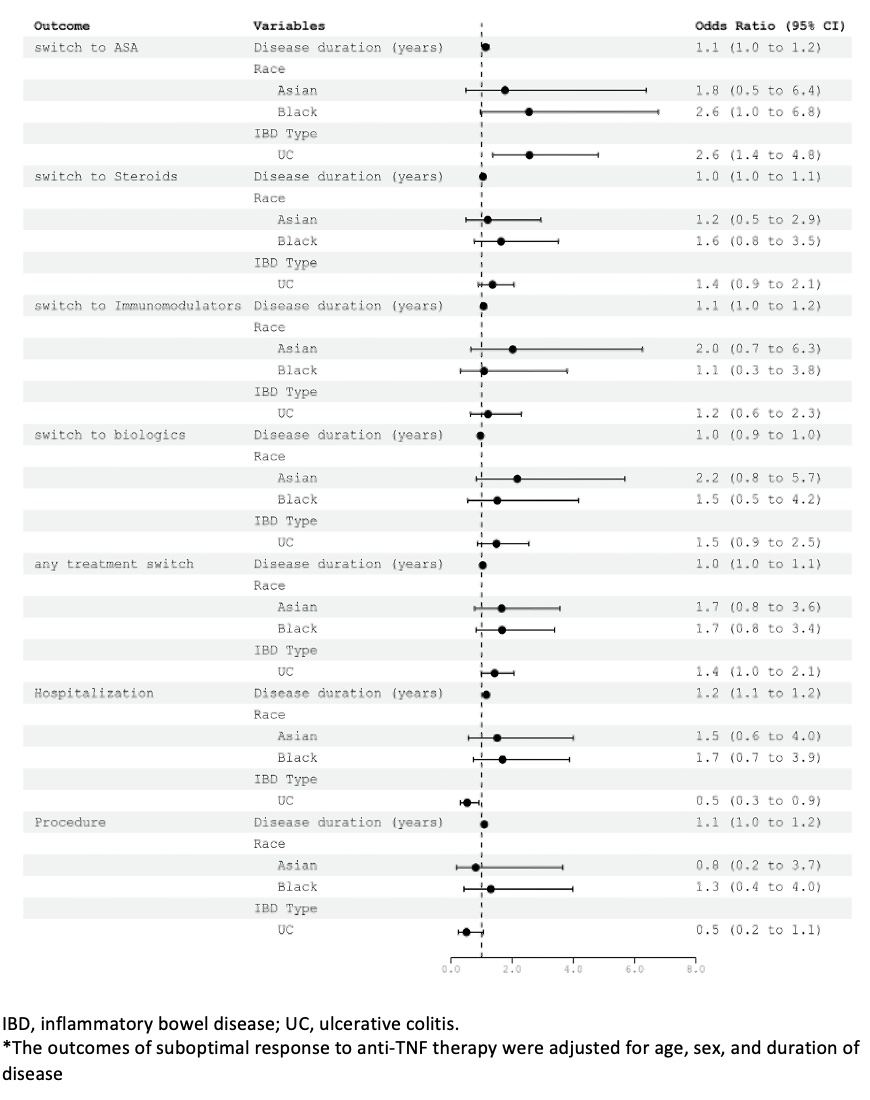
Figure: Figure 1. Adjusted odds ratios and confidence intervals of suboptimal response to anti-TNF therapy in Asian and Black patients compare to White patients with IBD. IBD, inflammatory bowel disease; CD, Crohn’s disease; UC, ulcerative colitis; Anti-TNF, anti-tumor necrosis factor; ASA, 5-amiosalicylate. aChi-square test; bFisher’s Exact Test.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jennifer Youn indicated no relevant financial relationships.
Ye Chen indicated no relevant financial relationships.
Sonia Friedman indicated no relevant financial relationships.
Jennifer Youn, MD1, Ye Chen, MSc1, Sonia Friedman, MD2. P0953 - Racial Differences in the Use of and Suboptimal Clinical Responses to Anti-TNF Therapy for Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
