Sunday Poster Session
Category: IBD
P0954 - Impact of Metabolic Syndrome on Ulcerative Colitis Patients and Their Cardiovascular Health: A Nationwide Cross-Sectional Analysis Using NIS
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SP
Sreeram Pannala, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Sai Shanmukha Sreeram Pannala, MD, Ryan Njeim, MD, Nadim Zaidan, MD, Liliane Deeb, MD
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Ulcerative Colitis (UC), as a chronic inflammatory disorder, is associated with an increased risk of heart diseases at a younger age and specifically during active flares. The presence of metabolic syndrome (MetS) and its components such as obesity, Diabetes Mellitus (DM), and hypertension (HTN) may complicate the picture and independently add to the risk of cardiovascular events in this context. By examining the interplay between UC and MetS, we aim to better understand the full scope of cardiovascular challenges in UC patients.
Methods: Utilizing NIS from 2016 to 2020, we extracted data for all hospitalized patients with a primary or secondary diagnosis of UC using ICD-10 codes. Inclusion criteria encompassed individuals older than 18 of all genders and races. We identified patients with metabolic syndrome within these inclusion criteria. We developed a calculated metabolic score (CMS), assigning a score of 1 for each of the 4 MetS criteria present (HTN, DM, dyslipidemia, obesity). Logistic regression was used to analyze cardiovascular outcomes in UC patients, adjusting to demographic variables such as age, gender, race, and CMS. Statistical analysis was performed using SAS 9.4.
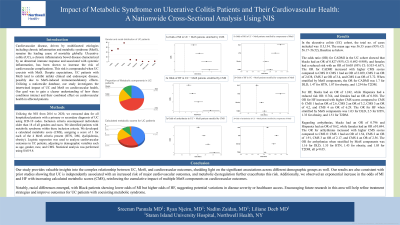
Results: 112,755 patients with UC were included over the 5-year period, with a mean age of 56.48 years. The odds of MI were 0.83 for blacks and 0.6 for females. When stratified by CMS, the OR for MI was 2 for a score of 1; 2.6 for a score of 2; 3.37 for a score of 3; and 3.68 for a score of 4 (p< 0.05). For heart failure (HF), the OR was 1.28 for blacks and 0.78 for Hispanics. Stratified by CMS, the OR for HF was 2.6 for a score of 1; 3.2 for a score of 2; 4.1 for a score of 3; and 6.2 for a score of 4 (p< 0.05). For arrhythmias, the OR was 0.69 for females, 0.78 for blacks, and 0.61 for Hispanics. Stratified by CMS, the OR for arrhythmias was 1.54 for a score of 1; 1.91 for a score of 2; 2.18 for a score of 3; and 2.58 for a score of 4 (p< 0.05).
Discussion: Our analysis demonstrates a significant association between UC and increased cardiovascular risks, particularly influenced by metabolic syndrome and its components. Notable variations were observed across genders and racial groups. A higher CMS score was significantly associated with multiple cardiovascular diseases. In conclusion, the CMS score seems to effectively stratify & emphasize the impact of metabolic factors on cardiovascular health in UC patients. Further RCTs are warranted to shed more light on this intricate association.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Shanmukha Sreeram Pannala, MD, Ryan Njeim, MD, Nadim Zaidan, MD, Liliane Deeb, MD. P0954 - Impact of Metabolic Syndrome on Ulcerative Colitis Patients and Their Cardiovascular Health: A Nationwide Cross-Sectional Analysis Using NIS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Ulcerative Colitis (UC), as a chronic inflammatory disorder, is associated with an increased risk of heart diseases at a younger age and specifically during active flares. The presence of metabolic syndrome (MetS) and its components such as obesity, Diabetes Mellitus (DM), and hypertension (HTN) may complicate the picture and independently add to the risk of cardiovascular events in this context. By examining the interplay between UC and MetS, we aim to better understand the full scope of cardiovascular challenges in UC patients.
Methods: Utilizing NIS from 2016 to 2020, we extracted data for all hospitalized patients with a primary or secondary diagnosis of UC using ICD-10 codes. Inclusion criteria encompassed individuals older than 18 of all genders and races. We identified patients with metabolic syndrome within these inclusion criteria. We developed a calculated metabolic score (CMS), assigning a score of 1 for each of the 4 MetS criteria present (HTN, DM, dyslipidemia, obesity). Logistic regression was used to analyze cardiovascular outcomes in UC patients, adjusting to demographic variables such as age, gender, race, and CMS. Statistical analysis was performed using SAS 9.4.
Results: 112,755 patients with UC were included over the 5-year period, with a mean age of 56.48 years. The odds of MI were 0.83 for blacks and 0.6 for females. When stratified by CMS, the OR for MI was 2 for a score of 1; 2.6 for a score of 2; 3.37 for a score of 3; and 3.68 for a score of 4 (p< 0.05). For heart failure (HF), the OR was 1.28 for blacks and 0.78 for Hispanics. Stratified by CMS, the OR for HF was 2.6 for a score of 1; 3.2 for a score of 2; 4.1 for a score of 3; and 6.2 for a score of 4 (p< 0.05). For arrhythmias, the OR was 0.69 for females, 0.78 for blacks, and 0.61 for Hispanics. Stratified by CMS, the OR for arrhythmias was 1.54 for a score of 1; 1.91 for a score of 2; 2.18 for a score of 3; and 2.58 for a score of 4 (p< 0.05).
Discussion: Our analysis demonstrates a significant association between UC and increased cardiovascular risks, particularly influenced by metabolic syndrome and its components. Notable variations were observed across genders and racial groups. A higher CMS score was significantly associated with multiple cardiovascular diseases. In conclusion, the CMS score seems to effectively stratify & emphasize the impact of metabolic factors on cardiovascular health in UC patients. Further RCTs are warranted to shed more light on this intricate association.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Ryan Njeim indicated no relevant financial relationships.
Nadim Zaidan indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala, MD, Ryan Njeim, MD, Nadim Zaidan, MD, Liliane Deeb, MD. P0954 - Impact of Metabolic Syndrome on Ulcerative Colitis Patients and Their Cardiovascular Health: A Nationwide Cross-Sectional Analysis Using NIS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
