Sunday Poster Session
Category: IBD
P0955 - Anticoagulation and Preprocedural Bleeding Risk in Patients with Inflammatory Bowel Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Veronica F. Williams, MD
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Veronica F. Williams, MD1, Jake S. Jasurda, DO1, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG1, Mary Moore, MS, MPH2
1Loyola University Medical Center, Maywood, IL; 2Loyola University Chicago, Clinical Research Office Biostatistics Collaborative Core, Maywood, IL
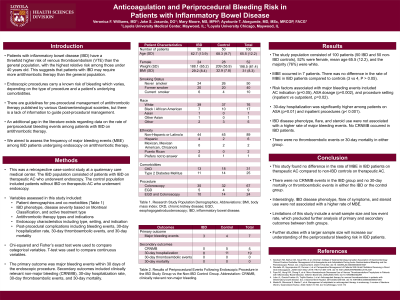
Introduction: Inflammatory bowel disease (IBD) patients on antithrombotic therapy are at risk of periprocedural bleeding during and after endoscopic procedures. However, there is a lack of data in the literature on the rate of periprocedural bleeding events among patients with IBD on antithrombotic therapy. We aimed to assess the frequency of major bleeding events (MBE) among IBD patients undergoing endoscopy on therapeutic anticoagulation (AC).
Methods: Retrospective case-control study at a quaternary care medical center. The IBD population consisted of patients with IBD on therapeutic AC who underwent endoscopy. The control population included patients without IBD on therapeutic AC who underwent endoscopy. The primary outcome was MBE within 30 days of the endoscopic procedure. Secondary outcomes included clinically relevant non-major bleeding (CRNMB), 30-day hospitalization rate, 30-day thromboembolic events, and 30-day mortality.
Results: The study population consisted of 100 patients (50 IBD and 50 non-IBD controls), 52% were female, mean age 65.5 (12.2), and the majority (76%) were white. MBE occurred in 7 patients. There was no difference in the rate of MBE in IBD patients compared to controls (3 vs 4, P > 0.05). Risk factors associated with major bleeding events included AC indication (p = 0.05), ASA dosage (p=0.002), and procedure setting (inpatient vs outpatient, p=0.02), 30-day hospitalization was significantly higher among patients on ASA (p=0.01) and inpatient procedures (p< 0.001). IBD disease phenotype, flare, or steroid use was not associated with a higher rate of major bleeding events. No CRNMB occurred in IBD patients. There were no thromboembolic events or 30-day mortality in either group.
Discussion: This study found no difference in the rate of MBE in IBD patients on therapeutic AC compared to non-IBD controls on therapeutic AC. There were no CRNMB events in the IBD group and no 30-day mortality or thromboembolic events in either the IBD or the control group. Interestingly, IBD disease phenotype, flare of symptoms, and steroid use were not associated with a higher rate of MBE. Limitations of this study included a small sample size and low event rate, which precluded further analysis of primary and secondary outcomes between both groups. Further studies with a larger sample size will increase our understanding of the periprocedural bleeding risk in IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Veronica F. Williams, MD1, Jake S. Jasurda, DO1, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG1, Mary Moore, MS, MPH2. P0955 - Anticoagulation and Preprocedural Bleeding Risk in Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Loyola University Chicago, Clinical Research Office Biostatistics Collaborative Core, Maywood, IL
Introduction: Inflammatory bowel disease (IBD) patients on antithrombotic therapy are at risk of periprocedural bleeding during and after endoscopic procedures. However, there is a lack of data in the literature on the rate of periprocedural bleeding events among patients with IBD on antithrombotic therapy. We aimed to assess the frequency of major bleeding events (MBE) among IBD patients undergoing endoscopy on therapeutic anticoagulation (AC).
Methods: Retrospective case-control study at a quaternary care medical center. The IBD population consisted of patients with IBD on therapeutic AC who underwent endoscopy. The control population included patients without IBD on therapeutic AC who underwent endoscopy. The primary outcome was MBE within 30 days of the endoscopic procedure. Secondary outcomes included clinically relevant non-major bleeding (CRNMB), 30-day hospitalization rate, 30-day thromboembolic events, and 30-day mortality.
Results: The study population consisted of 100 patients (50 IBD and 50 non-IBD controls), 52% were female, mean age 65.5 (12.2), and the majority (76%) were white. MBE occurred in 7 patients. There was no difference in the rate of MBE in IBD patients compared to controls (3 vs 4, P > 0.05). Risk factors associated with major bleeding events included AC indication (p = 0.05), ASA dosage (p=0.002), and procedure setting (inpatient vs outpatient, p=0.02), 30-day hospitalization was significantly higher among patients on ASA (p=0.01) and inpatient procedures (p< 0.001). IBD disease phenotype, flare, or steroid use was not associated with a higher rate of major bleeding events. No CRNMB occurred in IBD patients. There were no thromboembolic events or 30-day mortality in either group.
Discussion: This study found no difference in the rate of MBE in IBD patients on therapeutic AC compared to non-IBD controls on therapeutic AC. There were no CRNMB events in the IBD group and no 30-day mortality or thromboembolic events in either the IBD or the control group. Interestingly, IBD disease phenotype, flare of symptoms, and steroid use were not associated with a higher rate of MBE. Limitations of this study included a small sample size and low event rate, which precluded further analysis of primary and secondary outcomes between both groups. Further studies with a larger sample size will increase our understanding of the periprocedural bleeding risk in IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Veronica Williams indicated no relevant financial relationships.
Jake Jasurda indicated no relevant financial relationships.
Ayokunle Abegunde: Ferring Pharmaceuticals – Consultant. Ferring Pharmaceuticals – Consultant.
Mary Moore indicated no relevant financial relationships.
Veronica F. Williams, MD1, Jake S. Jasurda, DO1, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG1, Mary Moore, MS, MPH2. P0955 - Anticoagulation and Preprocedural Bleeding Risk in Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

