Sunday Poster Session
Category: IBD
P0871 - Prevalence of Clinically Significant Steatotic Liver Disease in Inflammatory Bowel Disease: A Prospective Evaluation Using Vibration Controlled Transient Elastography
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ujwala Pamidimukkala, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Ujwala Pamidimukkala, MD1, Justin Ceh, MD2, Elizabeth E. Williams, MD2, Tonika Peterson, 2, Debbie Drenzyk, 2, Sarah Pardue Brennan, 2, Rebecca A. Leonard, MS1, Monika Fischer, MD, MS2, Matthew Bohm, DO2, Raj Vuppalanchi, MD1, Naga Chalasani, MBBS2, Sashidhar Sagi, MD2
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN
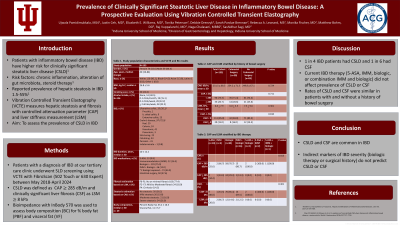
Introduction: Patients with inflammatory bowel disease (IBD) are at a higher risk for clinically significant steatotic liver disease (CSLD) due to chronic inflammation, alteration of the gut microbiota, and repeated or chronic exposure to steroid therapy. Studies have reported a wide range of prevalence of hepatic steatosis in IBD from 1.5% to 55%. Vibration Controlled Transient Elastography (VCTE) allows for simultaneous measurement of hepatic steatosis and fibrosis with controlled attenuation parameter (CAP) and liver stiffness measurement (LSM) respectively. We aimed to assess the prevalence of CSLD in patients with IBD.
Methods: Patients with an established diagnosis of IBD presenting to our tertiary care clinic were offered the opportunity to undergo screening for CSLD using VCTE with FibroScan (502 Touch or 630 Expert) between May 2018 and April 2024. CSLD was defined by a CAP ≥ 285 dB/m, and clinically significant liver fibrosis (CSF) was defined by an LSM ≥ 8 kPa. Bioimpedance using InBody 570 analyzer was used to assess body composition (BC) for percent body fat (PBF) and visceral fat (VF). All subjects provided informed consent for an IRB-approved protocol.
Results: A total of 133 subjects with IBD had a valid Fibroscan study with 36 (27%) of those also undergoing BC assessment. Study population characteristics and results of VCTE and BC are presented in Table 1. Of these participants, 2 individuals did not have a measured CAP. The prevalence of CSLD was 26.7% (35) and CSF was 15%(20). 3 subjects had advanced fibrosis (LSM >11.5 kPA) and 6 subjects had cirrhosis (LSM >14 kPa). Current IBD therapy (5-ASA, immunomodulator, biologic or combination biologic and immunomodulator therapy) did not affect the prevalence of CSLD (55.6% vs 44.4 %; 66.7% vs 33.3%; 70.7% vs 29.3%; 86.7% vs 13.3%; p=0.384) or CSF (80% vs 20%; 33.3%vs 66.7%;85.4 %vs 14.6 %; 87.5%vs 12.5%; p=0.237). The prevalence of CSLD [28.6% vs 25.6%, p=0.71] and CSF (16% vs 14.5%, p=0.810) were similar in IBD patients with and without a history of bowel surgery.
Discussion: In our cohort, approximately one in four IBD patients had CSLD while one in six had CSF. Indirect markers of IBD severity like biologic therapy or a history of bowel surgery did not predict the presence of CSLD or CSF
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ujwala Pamidimukkala, MD1, Justin Ceh, MD2, Elizabeth E. Williams, MD2, Tonika Peterson, 2, Debbie Drenzyk, 2, Sarah Pardue Brennan, 2, Rebecca A. Leonard, MS1, Monika Fischer, MD, MS2, Matthew Bohm, DO2, Raj Vuppalanchi, MD1, Naga Chalasani, MBBS2, Sashidhar Sagi, MD2. P0871 - Prevalence of Clinically Significant Steatotic Liver Disease in Inflammatory Bowel Disease: A Prospective Evaluation Using Vibration Controlled Transient Elastography, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN
Introduction: Patients with inflammatory bowel disease (IBD) are at a higher risk for clinically significant steatotic liver disease (CSLD) due to chronic inflammation, alteration of the gut microbiota, and repeated or chronic exposure to steroid therapy. Studies have reported a wide range of prevalence of hepatic steatosis in IBD from 1.5% to 55%. Vibration Controlled Transient Elastography (VCTE) allows for simultaneous measurement of hepatic steatosis and fibrosis with controlled attenuation parameter (CAP) and liver stiffness measurement (LSM) respectively. We aimed to assess the prevalence of CSLD in patients with IBD.
Methods: Patients with an established diagnosis of IBD presenting to our tertiary care clinic were offered the opportunity to undergo screening for CSLD using VCTE with FibroScan (502 Touch or 630 Expert) between May 2018 and April 2024. CSLD was defined by a CAP ≥ 285 dB/m, and clinically significant liver fibrosis (CSF) was defined by an LSM ≥ 8 kPa. Bioimpedance using InBody 570 analyzer was used to assess body composition (BC) for percent body fat (PBF) and visceral fat (VF). All subjects provided informed consent for an IRB-approved protocol.
Results: A total of 133 subjects with IBD had a valid Fibroscan study with 36 (27%) of those also undergoing BC assessment. Study population characteristics and results of VCTE and BC are presented in Table 1. Of these participants, 2 individuals did not have a measured CAP. The prevalence of CSLD was 26.7% (35) and CSF was 15%(20). 3 subjects had advanced fibrosis (LSM >11.5 kPA) and 6 subjects had cirrhosis (LSM >14 kPa). Current IBD therapy (5-ASA, immunomodulator, biologic or combination biologic and immunomodulator therapy) did not affect the prevalence of CSLD (55.6% vs 44.4 %; 66.7% vs 33.3%; 70.7% vs 29.3%; 86.7% vs 13.3%; p=0.384) or CSF (80% vs 20%; 33.3%vs 66.7%;85.4 %vs 14.6 %; 87.5%vs 12.5%; p=0.237). The prevalence of CSLD [28.6% vs 25.6%, p=0.71] and CSF (16% vs 14.5%, p=0.810) were similar in IBD patients with and without a history of bowel surgery.
Discussion: In our cohort, approximately one in four IBD patients had CSLD while one in six had CSF. Indirect markers of IBD severity like biologic therapy or a history of bowel surgery did not predict the presence of CSLD or CSF
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ujwala Pamidimukkala indicated no relevant financial relationships.
Justin Ceh indicated no relevant financial relationships.
Elizabeth Williams indicated no relevant financial relationships.
Tonika Peterson indicated no relevant financial relationships.
Debbie Drenzyk indicated no relevant financial relationships.
Sarah Pardue Brennan indicated no relevant financial relationships.
Rebecca Leonard indicated no relevant financial relationships.
Monika Fischer: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Eli Lilly and Company – Consultant. Ferring Pharmaceuticals – Consultant. Janssen – Consultant. Pfizer – Consultant. Rebiotix – Consultant. Scioto Biosciences – Consultant. Seres Therapeutics – Consultant.
Matthew Bohm indicated no relevant financial relationships.
Raj Vuppalanchi indicated no relevant financial relationships.
Naga Chalasani indicated no relevant financial relationships.
Sashidhar Sagi indicated no relevant financial relationships.
Ujwala Pamidimukkala, MD1, Justin Ceh, MD2, Elizabeth E. Williams, MD2, Tonika Peterson, 2, Debbie Drenzyk, 2, Sarah Pardue Brennan, 2, Rebecca A. Leonard, MS1, Monika Fischer, MD, MS2, Matthew Bohm, DO2, Raj Vuppalanchi, MD1, Naga Chalasani, MBBS2, Sashidhar Sagi, MD2. P0871 - Prevalence of Clinically Significant Steatotic Liver Disease in Inflammatory Bowel Disease: A Prospective Evaluation Using Vibration Controlled Transient Elastography, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
