Sunday Poster Session
Category: GI Bleeding
P0787 - A Fatal Case of Ectopic Variceal Hemorrhage in a Young Cirrhotic Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- ST
Shunsa Tarar, DO
Albany Medical Center
Albany, NY
Presenting Author(s)
Shunsa Tarar, DO1, Ahmad Abulawi, MD2, Neil Volk, MD1
1Albany Medical Center, Albany, NY; 2Albany Medical College, Albany, NY
Introduction: Ectopic varices rarely develop as a complication of portal hypertension in cirrhotic patients. Diagnosis is complicated by variance in variceal anatomy. Furthermore, ectopic variceal bleeding is a therapeutic challenge, necessitating endovascular intervention to control bleeding and thus associated with considerable mortality. We present a challenging case of rebleeding ectopic varices.
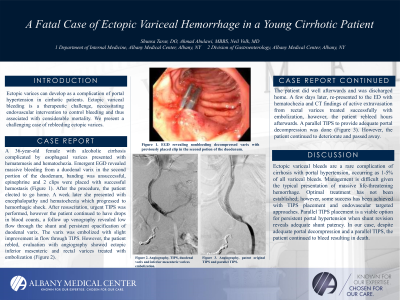
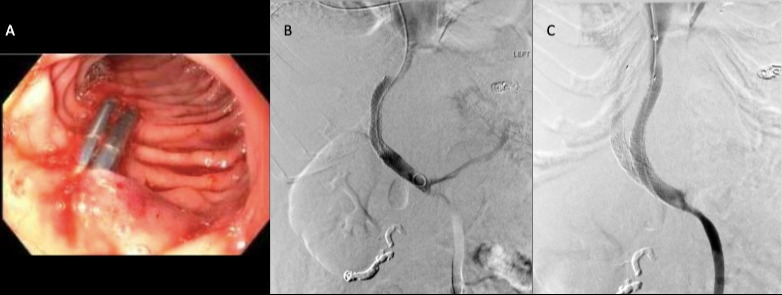
Case Description/Methods: A 36-year-old female with alcoholic cirrhosis complicated with esophageal varices presented with hematemesis and hematochezia. Emergent EGD revealed massive bleeding from a duodenal varix in the second portion of the duodenum, banding was unsuccessful, epinephrine and 2 clips were placed with successful hemostasis (Figure A). After the procedure, the patient elected to go home. A week later she presented with encephalopathy and hematochezia which progressed to hemorrhagic shock. After resuscitation the decision was made to proceed with urgent transjugular intrahepatic portosystemic shunt (TIPS), however the patient continued to have drops in blood counts, a follow up venography revealed low flow through the shunt and persistent opacification of duodenal varix. The varix was embolized with slight improvement in flow through TIPS. However, the patient rebled, evaluation with angiography showed ectopic inferior mesenteric and rectal varices treated with embolization (Figure B). The patient did well afterwards and was discharged home. A few days later, returned to the ED with hematochezia and CT findings of active extravasation from rectal varices treated successfully with embolization, however, the patient rebleed hours afterwards. Decision was made to proceed with a parallel TIPS to provide adequate portal decompression (Figure C). However, the patient continued to deteriorate and passed away.
Discussion: Ectopic variceal bleeds are a rare complication of cirrhosis with portal hypertension, occurring as 1-5% of all variceal bleeds. Management is difficult given the challenge in establishing a diagnosis and typical presentation of massive life-threatening hemorrhage. Optimal treatment has not been established; however, some success has been achieved with TIPS placement and endovascular targeted approaches. Parallel TIPS placement is a viable option for persistent portal hypertension when shunt revision reveals adequate shunt patency. In our case, despite adequate portal decompression and a parallel TIPS, the patient continued to bleed resulting in death.
Disclosures:
Shunsa Tarar, DO1, Ahmad Abulawi, MD2, Neil Volk, MD1. P0787 - A Fatal Case of Ectopic Variceal Hemorrhage in a Young Cirrhotic Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albany Medical Center, Albany, NY; 2Albany Medical College, Albany, NY
Introduction: Ectopic varices rarely develop as a complication of portal hypertension in cirrhotic patients. Diagnosis is complicated by variance in variceal anatomy. Furthermore, ectopic variceal bleeding is a therapeutic challenge, necessitating endovascular intervention to control bleeding and thus associated with considerable mortality. We present a challenging case of rebleeding ectopic varices.
Case Description/Methods: A 36-year-old female with alcoholic cirrhosis complicated with esophageal varices presented with hematemesis and hematochezia. Emergent EGD revealed massive bleeding from a duodenal varix in the second portion of the duodenum, banding was unsuccessful, epinephrine and 2 clips were placed with successful hemostasis (Figure A). After the procedure, the patient elected to go home. A week later she presented with encephalopathy and hematochezia which progressed to hemorrhagic shock. After resuscitation the decision was made to proceed with urgent transjugular intrahepatic portosystemic shunt (TIPS), however the patient continued to have drops in blood counts, a follow up venography revealed low flow through the shunt and persistent opacification of duodenal varix. The varix was embolized with slight improvement in flow through TIPS. However, the patient rebled, evaluation with angiography showed ectopic inferior mesenteric and rectal varices treated with embolization (Figure B). The patient did well afterwards and was discharged home. A few days later, returned to the ED with hematochezia and CT findings of active extravasation from rectal varices treated successfully with embolization, however, the patient rebleed hours afterwards. Decision was made to proceed with a parallel TIPS to provide adequate portal decompression (Figure C). However, the patient continued to deteriorate and passed away.
Discussion: Ectopic variceal bleeds are a rare complication of cirrhosis with portal hypertension, occurring as 1-5% of all variceal bleeds. Management is difficult given the challenge in establishing a diagnosis and typical presentation of massive life-threatening hemorrhage. Optimal treatment has not been established; however, some success has been achieved with TIPS placement and endovascular targeted approaches. Parallel TIPS placement is a viable option for persistent portal hypertension when shunt revision reveals adequate shunt patency. In our case, despite adequate portal decompression and a parallel TIPS, the patient continued to bleed resulting in death.
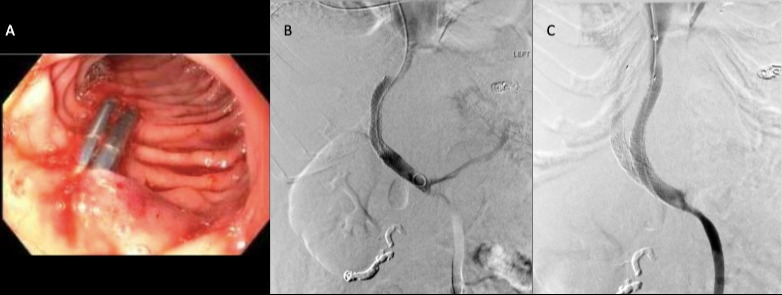
Figure: Figure 1: EGD revealing non-bleeding decompressed varix with previously placed clip in the second potion of the duodenum (A). Angiography showing TIPS, duodenal varix and inferior mesenteric varices embolization (B). Angiography showing patent original TIPS and parallel TIPS (C).
Disclosures:
Shunsa Tarar indicated no relevant financial relationships.
Ahmad Abulawi indicated no relevant financial relationships.
Neil Volk indicated no relevant financial relationships.
Shunsa Tarar, DO1, Ahmad Abulawi, MD2, Neil Volk, MD1. P0787 - A Fatal Case of Ectopic Variceal Hemorrhage in a Young Cirrhotic Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
