Sunday Poster Session
Category: GI Bleeding
P0791 - The Perpetual Hemorrhage: Managing Recurrent Gastrointestinal Bleeding in Hereditary Hemorrhagic Telangiectasia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KT
Kimberly Tena Diaz, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Kimberly Tena Diaz, DO1, Kathy N. Williams, MD, MS2, Apeksha Shah, MD3, Adib Chaaya, MD4, Tonia Liu, BS5
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Philadelphia, PA; 3Digestive Health Institute at Cooper University Hospital, Mt. Laurel, NJ; 4Cooper Health Gastroenterology, Camden, NJ; 5Cooper Medical School of Rowan University, Deptford, NJ
Introduction: Hereditary hemorrhagic Telangiectasia (HHT) is a genetic disorder that leads to arteriovenous malformations (AVMs) partly due to the lack of capillaries. HHT has an age-related penetrance with progressive AVM formations that may form anywhere, but most often form in the nasal, pulmonary, hepatic or cerebral circulation. Despite this, 15-20% of patients with HHT experience recurrent gastrointestinal (GI) bleeding. Our aim is to bring awareness to treatment options in a patient with HHT and recurrent GI AVM bleeding.
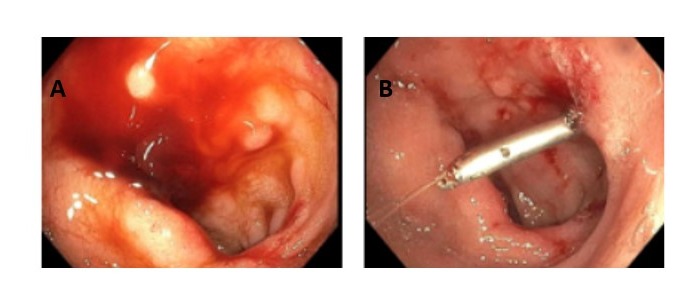
Case Description/Methods: We present a 62-year-old male with medical history of HHT complicated by recurrent GI bleeding and chronic anemia. Outpatient management included iron supplementation, intravenous iron infusions, and hemoglobin checks. In one year, he was admitted to the hospital eight times due to critically low hemoglobin detected in outpatient labs. On his first admission, push enteroscopy revealed multiple nonbleeding and bleeding AVMs in the esophagus, stomach, jejunum, and duodenum. These were treated with Argon plasma coagulation (APC) and endoclips were placed in the duodenal AVM. He received multiple units of packed red blood cells and was discharged. One month later, he was readmitted for a similar presentation and again required multiple transfusions. Push enteroscopy showed similar results from his previous procedure so he underwent APC and endoclip placement. Of note, hemolysis labs were negative. Once stable, he was discharged home and continued his outpatient regimen. He returned to the hospital after outpatient labs revealed hemoglobin of 5.2. Repeat push enteroscopy revealed eroded mucosa and both bleeding and non-bleeding AVMs in the same areas as his first procedure, again treated with APC. He returned to his outpatient hematologist who recommended initiating bevacizumab.
Discussion: Patients with HHT may experience epistaxis, hemoptysis, liver cirrhosis or recurrent GI bleeding due to AVM formation. The pathogenesis of HHT includes increased vascular endothelial growth factor (VEGF) expression causing aberrant angiogenesis. Endoscopic interventions may offer earlier detection of GI AVMs but may be futile in treating patients with HHT and recurrent GI bleeding as seen in our patient. One randomized control trial in 2023 found that in patients such as ours, using bevacizumab, an anti-VEGF antibody, may lead to patients requiring less transfusions. Thus, this treatment should be considered when other options such as endoscopic interventions have failed.
Disclosures:
Kimberly Tena Diaz, DO1, Kathy N. Williams, MD, MS2, Apeksha Shah, MD3, Adib Chaaya, MD4, Tonia Liu, BS5. P0791 - The Perpetual Hemorrhage: Managing Recurrent Gastrointestinal Bleeding in Hereditary Hemorrhagic Telangiectasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Philadelphia, PA; 3Digestive Health Institute at Cooper University Hospital, Mt. Laurel, NJ; 4Cooper Health Gastroenterology, Camden, NJ; 5Cooper Medical School of Rowan University, Deptford, NJ
Introduction: Hereditary hemorrhagic Telangiectasia (HHT) is a genetic disorder that leads to arteriovenous malformations (AVMs) partly due to the lack of capillaries. HHT has an age-related penetrance with progressive AVM formations that may form anywhere, but most often form in the nasal, pulmonary, hepatic or cerebral circulation. Despite this, 15-20% of patients with HHT experience recurrent gastrointestinal (GI) bleeding. Our aim is to bring awareness to treatment options in a patient with HHT and recurrent GI AVM bleeding.
Case Description/Methods: We present a 62-year-old male with medical history of HHT complicated by recurrent GI bleeding and chronic anemia. Outpatient management included iron supplementation, intravenous iron infusions, and hemoglobin checks. In one year, he was admitted to the hospital eight times due to critically low hemoglobin detected in outpatient labs. On his first admission, push enteroscopy revealed multiple nonbleeding and bleeding AVMs in the esophagus, stomach, jejunum, and duodenum. These were treated with Argon plasma coagulation (APC) and endoclips were placed in the duodenal AVM. He received multiple units of packed red blood cells and was discharged. One month later, he was readmitted for a similar presentation and again required multiple transfusions. Push enteroscopy showed similar results from his previous procedure so he underwent APC and endoclip placement. Of note, hemolysis labs were negative. Once stable, he was discharged home and continued his outpatient regimen. He returned to the hospital after outpatient labs revealed hemoglobin of 5.2. Repeat push enteroscopy revealed eroded mucosa and both bleeding and non-bleeding AVMs in the same areas as his first procedure, again treated with APC. He returned to his outpatient hematologist who recommended initiating bevacizumab.
Discussion: Patients with HHT may experience epistaxis, hemoptysis, liver cirrhosis or recurrent GI bleeding due to AVM formation. The pathogenesis of HHT includes increased vascular endothelial growth factor (VEGF) expression causing aberrant angiogenesis. Endoscopic interventions may offer earlier detection of GI AVMs but may be futile in treating patients with HHT and recurrent GI bleeding as seen in our patient. One randomized control trial in 2023 found that in patients such as ours, using bevacizumab, an anti-VEGF antibody, may lead to patients requiring less transfusions. Thus, this treatment should be considered when other options such as endoscopic interventions have failed.
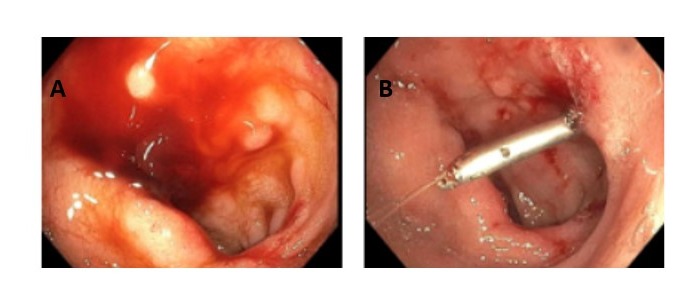
Figure: Figure A: Active AVM bleeding in duodenal bulb
Figure B: Clip placement with cessation of AVM bleeding in duodenal bulb
Figure B: Clip placement with cessation of AVM bleeding in duodenal bulb
Disclosures:
Kimberly Tena Diaz indicated no relevant financial relationships.
Kathy Williams indicated no relevant financial relationships.
Apeksha Shah indicated no relevant financial relationships.
Adib Chaaya indicated no relevant financial relationships.
Tonia Liu indicated no relevant financial relationships.
Kimberly Tena Diaz, DO1, Kathy N. Williams, MD, MS2, Apeksha Shah, MD3, Adib Chaaya, MD4, Tonia Liu, BS5. P0791 - The Perpetual Hemorrhage: Managing Recurrent Gastrointestinal Bleeding in Hereditary Hemorrhagic Telangiectasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
