Sunday Poster Session
Category: GI Bleeding
P0793 - Splenic Variceal Bleeding Presenting With Hemorrhagic Shock in Cirrhosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Fatma Ozguc, DO
UTHSCSA
San Antonio, TX
Presenting Author(s)
Fatma Ozguc, DO1, Sylvia Keiser, DO1, Jawairia Memon, MD2, Chandraprakash Umapathy, MD3
1UTHSCSA, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3University of Texas Health San Antonio, San Antonio, TX
Introduction: Portal hypertension, often caused by advanced cirrhosis, results in collateral vessels that bypass the liver. These collaterals, or varices, particularly in the esophagus and stomach, can be prone to bleeding. Splenic varices are rare and associated with conditions leading to splenic vein thrombosis (SVT) or left-sided portal hypertension1. Here, we present a case of hemorrhagic shock caused by splenic variceal bleeding in a cirrhotic patient.
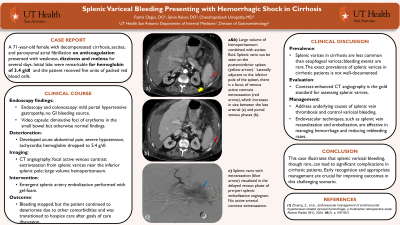
Case Description/Methods: A 71-year-old female with decompensated cirrhosis with ascites and paroxysmal atrial fibrillation on anticoagulation presented to the emergency room with weakness, dizziness, and melenic stools for several days. Her hemoglobin was found to be 3.4 g/dl, and she received five units of packed red blood cells. Endoscopy and colonoscopy revealed mild portal hypertensive gastropathy but no sources of gastrointestinal (GI) bleeding. A video capsule endoscopy showed diminutive foci of erythema in the small bowel but otherwise normal. The same day, the patient decompensated with acute abdominal pain, severe hypotension, tachycardia, and a drop in hemoglobin to 5.4 g/dl. Emergent computed tomography (CT) angiography showed focal active venous contrast extravasation from splenic varices adjacent to the inferior splenic pole, associated with a large volume hemoperitoneum. The splenic artery was emergently embolized by interventional radiology. Although the bleeding stopped, the patient continued to deteriorate despite resuscitative measures due to other comorbidities and was eventually transitioned to hospice care after discussing goals of care.
Discussion: The prevalence of splenic varices in cirrhosis in comparison to esophageal varices is not well defined, and splenic variceal bleeding in cirrhosis is rare in the literature. Contrast-enhanced CT angiography is the gold standard for evaluating splenic varices1. The management involves addressing the underlying cause of SVT and controlling the variceal bleeding1. Endovascular techniques, such as splenic vein recanalization and embolization, have also shown promise in managing variceal hemorrhage and reducing rebleeding rates1. Splenic varices should be suspected in cirrhotic patients who present with clinically significant bleeding with hemodynamic instability in the setting of a negative initial work-up.
[1]Zhuang, Z., et al., Endovascular management of sinistral portal hypertension-related variceal hemorrhage: a multicenter retrospective study. Abdom Radiol (NY), 2024. 49(2): p. 597-603
Disclosures:
Fatma Ozguc, DO1, Sylvia Keiser, DO1, Jawairia Memon, MD2, Chandraprakash Umapathy, MD3. P0793 - Splenic Variceal Bleeding Presenting With Hemorrhagic Shock in Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UTHSCSA, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3University of Texas Health San Antonio, San Antonio, TX
Introduction: Portal hypertension, often caused by advanced cirrhosis, results in collateral vessels that bypass the liver. These collaterals, or varices, particularly in the esophagus and stomach, can be prone to bleeding. Splenic varices are rare and associated with conditions leading to splenic vein thrombosis (SVT) or left-sided portal hypertension1. Here, we present a case of hemorrhagic shock caused by splenic variceal bleeding in a cirrhotic patient.
Case Description/Methods: A 71-year-old female with decompensated cirrhosis with ascites and paroxysmal atrial fibrillation on anticoagulation presented to the emergency room with weakness, dizziness, and melenic stools for several days. Her hemoglobin was found to be 3.4 g/dl, and she received five units of packed red blood cells. Endoscopy and colonoscopy revealed mild portal hypertensive gastropathy but no sources of gastrointestinal (GI) bleeding. A video capsule endoscopy showed diminutive foci of erythema in the small bowel but otherwise normal. The same day, the patient decompensated with acute abdominal pain, severe hypotension, tachycardia, and a drop in hemoglobin to 5.4 g/dl. Emergent computed tomography (CT) angiography showed focal active venous contrast extravasation from splenic varices adjacent to the inferior splenic pole, associated with a large volume hemoperitoneum. The splenic artery was emergently embolized by interventional radiology. Although the bleeding stopped, the patient continued to deteriorate despite resuscitative measures due to other comorbidities and was eventually transitioned to hospice care after discussing goals of care.
Discussion: The prevalence of splenic varices in cirrhosis in comparison to esophageal varices is not well defined, and splenic variceal bleeding in cirrhosis is rare in the literature. Contrast-enhanced CT angiography is the gold standard for evaluating splenic varices1. The management involves addressing the underlying cause of SVT and controlling the variceal bleeding1. Endovascular techniques, such as splenic vein recanalization and embolization, have also shown promise in managing variceal hemorrhage and reducing rebleeding rates1. Splenic varices should be suspected in cirrhotic patients who present with clinically significant bleeding with hemodynamic instability in the setting of a negative initial work-up.
[1]Zhuang, Z., et al., Endovascular management of sinistral portal hypertension-related variceal hemorrhage: a multicenter retrospective study. Abdom Radiol (NY), 2024. 49(2): p. 597-603
Disclosures:
Fatma Ozguc indicated no relevant financial relationships.
Sylvia Keiser indicated no relevant financial relationships.
Jawairia Memon indicated no relevant financial relationships.
Chandraprakash Umapathy indicated no relevant financial relationships.
Fatma Ozguc, DO1, Sylvia Keiser, DO1, Jawairia Memon, MD2, Chandraprakash Umapathy, MD3. P0793 - Splenic Variceal Bleeding Presenting With Hemorrhagic Shock in Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
