Sunday Poster Session
Category: GI Bleeding
P0799 - Tacrolimus-Induced Acute Esophageal Necrosis Post Orthotopic Liver Transplantation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Makeda Dawkins, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Makeda Dawkins, MD, Kenji Okumura, MD, Joon Sub Lee, BS, Nao Hara, MD, PhD, Fouzia Shakil, MBBS, PhD, Roxana Bodin, MD, Shireen Pais, MBBS, Abhay Dhand, MD, Seigo Nishida, MD, PhD
Westchester Medical Center, Valhalla, NY
Introduction: Acute esophageal necrosis (AEN) is a rare cause of gastrointestinal bleeding, characterized by circumferential esophageal necrosis sparing the gastroesophageal junction (GEJ), and is thought to be caused by a combination of an ischemic insult and erosive topic injury. We present a unique case of tacrolimus induced AEN in a liver transplant recipient, marking a potential adverse effect of a commonly used immunosuppressive agent.
Case Description/Methods: A 54-year-old male with liver transplantation was transitioned from tacrolimus to cyclosporine due to acute kidney injury and altered mentation during the immediate post-transplant period. Two weeks later allograft rejection was clinically suspected after he developed mild transaminitis. Cyclosporine was discontinued and prednisone and tacrolimus were restarted, with resolution of transaminitis. Two months later, he
presented
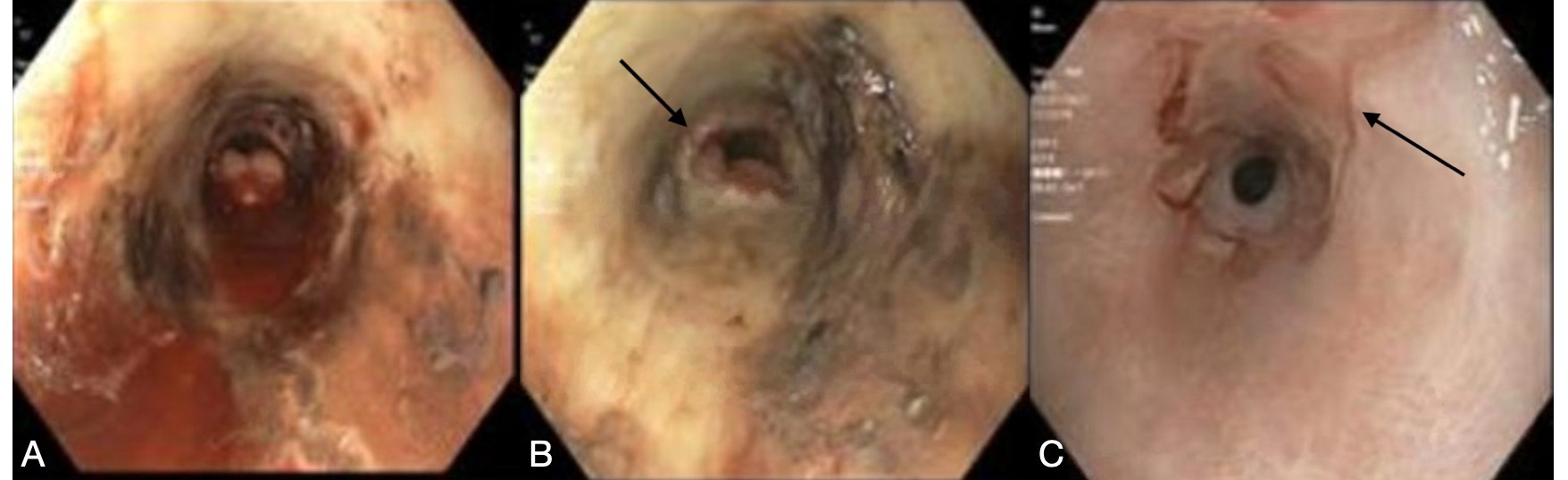
with dysphagia and intermittent hematochezia for two weeks. Esophagogastroduodenoscopy (EGD) showed diffuse esophageal necrosis, mucosal ulcerations, friability, and blackening sparing the GEJ (Figure A, B), confirming AEN. In absence of other underlying etiologies associated with AEN, tacrolimus was stopped and replaced with cyclosporine. Supportive care was initiated with intravenous resuscitation, high-dose pantoprazole, and NPO restriction. His symptoms gradually improved over one week. Repeat EGD was performed at three months for dysphagia, showing resolution of necrotizing esophagitis with residual ulceration of the middle-to-distal esophagus (Figure C). A new mid-esophageal stricture was noted, requiring stepwise balloon dilation. He remained symptom-free at one-year follow-up.
Discussion: While AEN has been previously described in patients with profound systemic hypoperfusion, severe topical esophageal injury, or with use of vasoconstricting antihypertensives, this is the first case of tacrolimus-induced acute esophageal necrosis without any preceding hemodynamic compromise. Tacrolimus is associated with cellular apoptosis and mucosal destruction in various organs without any chronological correlation to duration of treatment. A similar pattern of injury may be implicated in tacrolimus-induced AEN either by drug-related immune dysregulation or endothelial damage via local vasoconstriction. This case highlights the need for pharmacovigilance and a high index of suspicion for tacrolimus induced AEN in transplant recipients who may present with unexplained gastrointestinal bleeding.
Disclosures:
Makeda Dawkins, MD, Kenji Okumura, MD, Joon Sub Lee, BS, Nao Hara, MD, PhD, Fouzia Shakil, MBBS, PhD, Roxana Bodin, MD, Shireen Pais, MBBS, Abhay Dhand, MD, Seigo Nishida, MD, PhD. P0799 - Tacrolimus-Induced Acute Esophageal Necrosis Post Orthotopic Liver Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Acute esophageal necrosis (AEN) is a rare cause of gastrointestinal bleeding, characterized by circumferential esophageal necrosis sparing the gastroesophageal junction (GEJ), and is thought to be caused by a combination of an ischemic insult and erosive topic injury. We present a unique case of tacrolimus induced AEN in a liver transplant recipient, marking a potential adverse effect of a commonly used immunosuppressive agent.
Case Description/Methods: A 54-year-old male with liver transplantation was transitioned from tacrolimus to cyclosporine due to acute kidney injury and altered mentation during the immediate post-transplant period. Two weeks later allograft rejection was clinically suspected after he developed mild transaminitis. Cyclosporine was discontinued and prednisone and tacrolimus were restarted, with resolution of transaminitis. Two months later, he
presented
with dysphagia and intermittent hematochezia for two weeks. Esophagogastroduodenoscopy (EGD) showed diffuse esophageal necrosis, mucosal ulcerations, friability, and blackening sparing the GEJ (Figure A, B), confirming AEN. In absence of other underlying etiologies associated with AEN, tacrolimus was stopped and replaced with cyclosporine. Supportive care was initiated with intravenous resuscitation, high-dose pantoprazole, and NPO restriction. His symptoms gradually improved over one week. Repeat EGD was performed at three months for dysphagia, showing resolution of necrotizing esophagitis with residual ulceration of the middle-to-distal esophagus (Figure C). A new mid-esophageal stricture was noted, requiring stepwise balloon dilation. He remained symptom-free at one-year follow-up.
Discussion: While AEN has been previously described in patients with profound systemic hypoperfusion, severe topical esophageal injury, or with use of vasoconstricting antihypertensives, this is the first case of tacrolimus-induced acute esophageal necrosis without any preceding hemodynamic compromise. Tacrolimus is associated with cellular apoptosis and mucosal destruction in various organs without any chronological correlation to duration of treatment. A similar pattern of injury may be implicated in tacrolimus-induced AEN either by drug-related immune dysregulation or endothelial damage via local vasoconstriction. This case highlights the need for pharmacovigilance and a high index of suspicion for tacrolimus induced AEN in transplant recipients who may present with unexplained gastrointestinal bleeding.
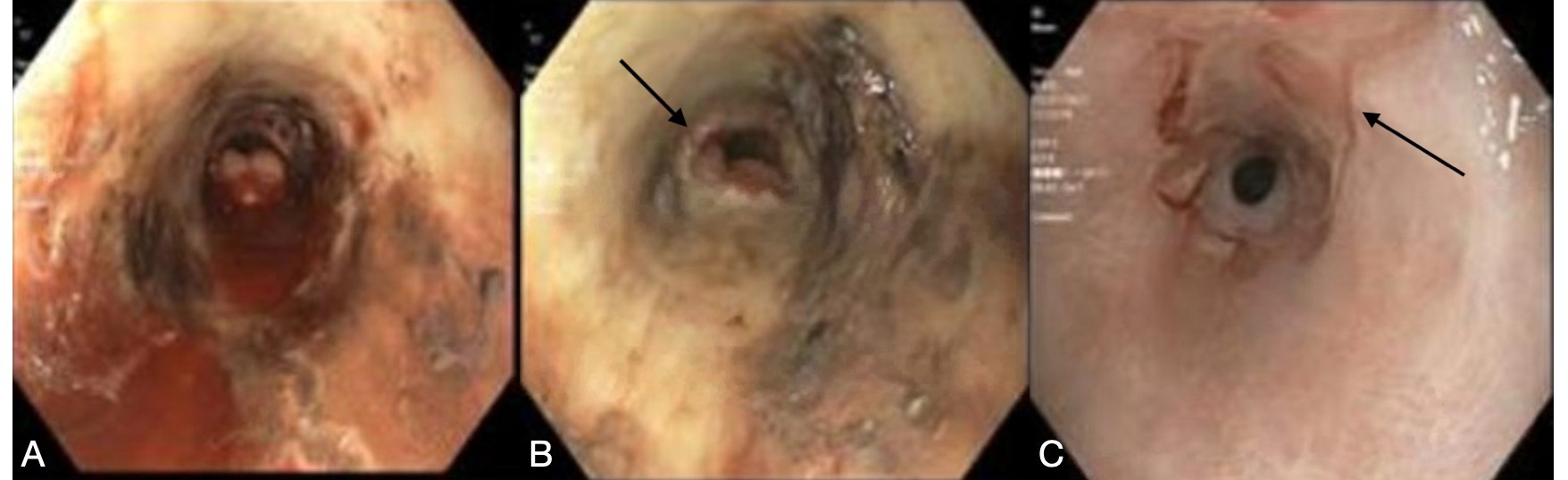
Figure: Figure 1: Acute esophageal necrosis (A) Endoscopic view of the mid esophagus showing circumferential erythema, friability, necrosis and active bleeding extending caudally to the distal esophagus with sharp demarcation at the gastroesophageal junction (B). Interval endoscopic assessment three months later with residual longitudinal ulceration and (C) a distal esophageal stricture.
Disclosures:
Makeda Dawkins indicated no relevant financial relationships.
Kenji Okumura indicated no relevant financial relationships.
Joon Sub Lee indicated no relevant financial relationships.
Nao Hara indicated no relevant financial relationships.
Fouzia Shakil indicated no relevant financial relationships.
Roxana Bodin indicated no relevant financial relationships.
Shireen Pais indicated no relevant financial relationships.
Abhay Dhand indicated no relevant financial relationships.
Seigo Nishida indicated no relevant financial relationships.
Makeda Dawkins, MD, Kenji Okumura, MD, Joon Sub Lee, BS, Nao Hara, MD, PhD, Fouzia Shakil, MBBS, PhD, Roxana Bodin, MD, Shireen Pais, MBBS, Abhay Dhand, MD, Seigo Nishida, MD, PhD. P0799 - Tacrolimus-Induced Acute Esophageal Necrosis Post Orthotopic Liver Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
