Sunday Poster Session
Category: GI Bleeding
P0800 - Sinister Sequalae – A Rare Case of Left Sided Portal Hypertension
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Brysen Keith, DO, MSBE
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Brysen Keith, DO, MSBE, Neal Viradia, MD, MPH
University of Miami Miller School of Medicine, Miami, FL
Introduction: Gastric varices most commonly occur as a result of cirrhosis or portal vein thrombosis causing portal hypertension and the formation of portosystemic shunts. Less commonly, portal hypertension can arise from pancreatic or splenic pathology resulting in left-side or sinistral portal hypertension (SPH). Here we describe a case of sinistral portal hypertension resulting from primary pancreatic malignancy complicated by splenic vein thrombosis.
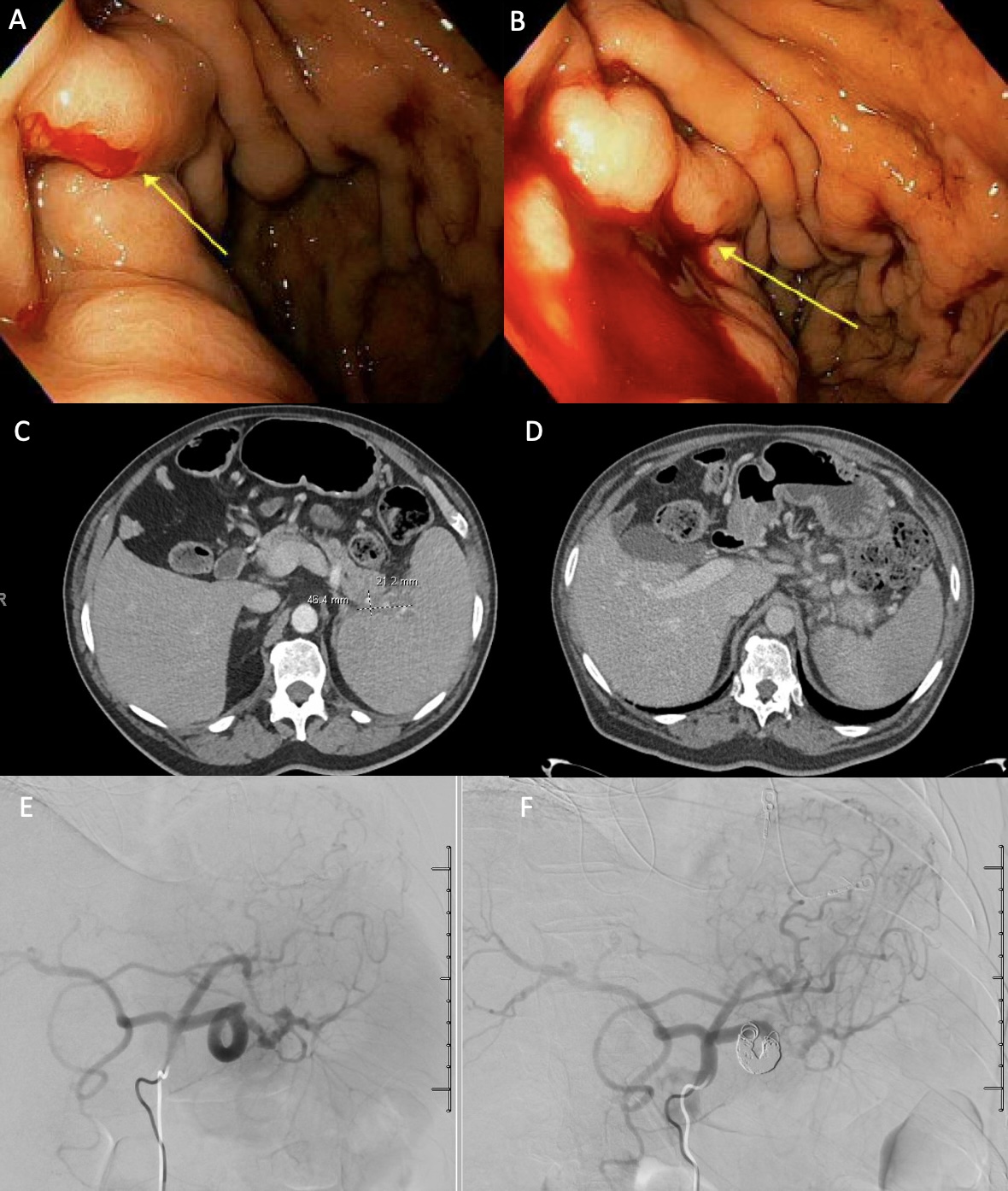
Case Description/Methods: 70-year-old male with a past medical history of pancreatic tail adenocarcinoma with abdominal metastasis who presented for outpatient upper endoscopy after he was noted to have worsening iron deficiency anemia requiring transfusions and two weeks of melena associated with fatigue and dizziness. Upper endoscopy was significant for an active gastric variceal bleed refractory to endoscopic management. Interventional Radiology (IR) was then consulted for Transjugular Intrahepatic Portosystemic Shunt (TIPS) vs Balloon-Occluded Retrograde Transverse Obliteration. Review of prior imaging was notable splenic vein thrombosis, likely from known pancreatic mass, without evidence of cirrhosis or esophageal varices. Patient then underwent emergent coil embolization of the proximal splenic artery by IR. Following the procedure, the patient had resolution of his melena and stabilization of his Hgb. Repeat CTA 1 month later showed improvement in gastric varices.
Discussion: SPH can occur in any splenic or pancreatic pathology with acute or chronic pancreatitis being the most common. This case highlights the importance of being aware of the less common causes for gastric variceal bleeding (GVB), especially in patients with known splenic or pancreatic pathology and/or a lack of chronic liver disease as gastric bleeding from SPH can be fatal. Gastric varices are most commonly secondary to splenorenal shunts typically treated with TIPS or BRTO. In this case, the gastric varices were due to splenic vein thrombosis causing elevated left-sided pressures so a TIPS or BRTO would provide no clinical benefit. In cases where splenic artery embolization is indicated, there are no reported cases of patients experiencing variceal rebleeding. Splenectomy or splenic artery embolization is the treatment of choice for GVB. For patients without GVB conservative treatment is preferred.
Disclosures:
Brysen Keith, DO, MSBE, Neal Viradia, MD, MPH. P0800 - Sinister Sequalae – A Rare Case of Left Sided Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Miami Miller School of Medicine, Miami, FL
Introduction: Gastric varices most commonly occur as a result of cirrhosis or portal vein thrombosis causing portal hypertension and the formation of portosystemic shunts. Less commonly, portal hypertension can arise from pancreatic or splenic pathology resulting in left-side or sinistral portal hypertension (SPH). Here we describe a case of sinistral portal hypertension resulting from primary pancreatic malignancy complicated by splenic vein thrombosis.
Case Description/Methods: 70-year-old male with a past medical history of pancreatic tail adenocarcinoma with abdominal metastasis who presented for outpatient upper endoscopy after he was noted to have worsening iron deficiency anemia requiring transfusions and two weeks of melena associated with fatigue and dizziness. Upper endoscopy was significant for an active gastric variceal bleed refractory to endoscopic management. Interventional Radiology (IR) was then consulted for Transjugular Intrahepatic Portosystemic Shunt (TIPS) vs Balloon-Occluded Retrograde Transverse Obliteration. Review of prior imaging was notable splenic vein thrombosis, likely from known pancreatic mass, without evidence of cirrhosis or esophageal varices. Patient then underwent emergent coil embolization of the proximal splenic artery by IR. Following the procedure, the patient had resolution of his melena and stabilization of his Hgb. Repeat CTA 1 month later showed improvement in gastric varices.
Discussion: SPH can occur in any splenic or pancreatic pathology with acute or chronic pancreatitis being the most common. This case highlights the importance of being aware of the less common causes for gastric variceal bleeding (GVB), especially in patients with known splenic or pancreatic pathology and/or a lack of chronic liver disease as gastric bleeding from SPH can be fatal. Gastric varices are most commonly secondary to splenorenal shunts typically treated with TIPS or BRTO. In this case, the gastric varices were due to splenic vein thrombosis causing elevated left-sided pressures so a TIPS or BRTO would provide no clinical benefit. In cases where splenic artery embolization is indicated, there are no reported cases of patients experiencing variceal rebleeding. Splenectomy or splenic artery embolization is the treatment of choice for GVB. For patients without GVB conservative treatment is preferred.
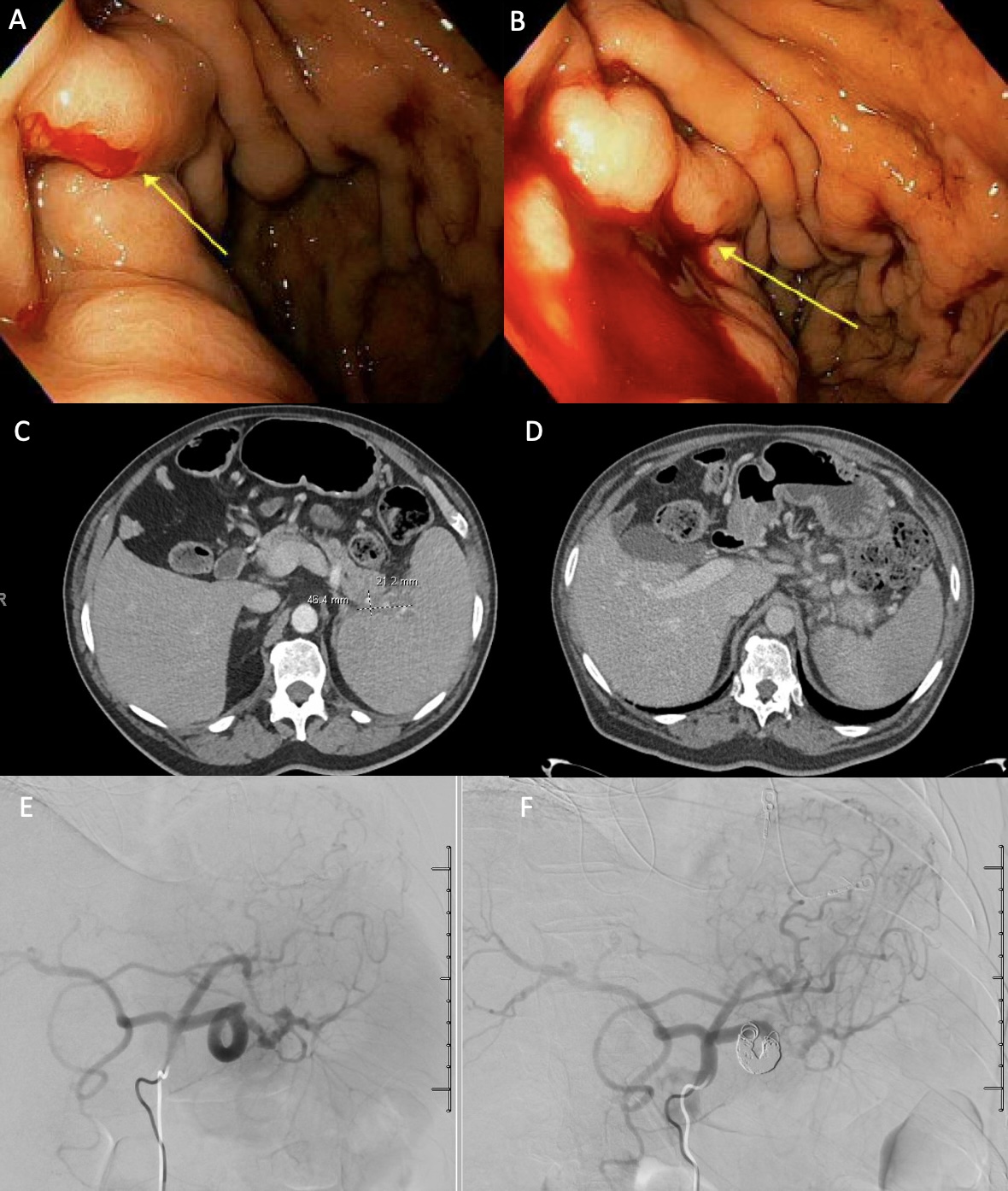
Figure: Figure A&B: Upper endoscopy showing an active variceal bleed in the gastric fundus. Figure C: CT with contrast showing ill-defined pancreatic tail mass extending to the splenic hilum with evidence of chronic splenic vein thrombosis with perisplenic, gastric, and mesenteric collaterals. Figure D: CT post-embolization showing stable embolization with improvement in varices and wedge-shaped hypodensities in the posterior aspect of the spleen. Figure E&F: Splenic angiogram pre (E) and post (F) proximal splenic artery coil embolization.
Disclosures:
Brysen Keith indicated no relevant financial relationships.
Neal Viradia indicated no relevant financial relationships.
Brysen Keith, DO, MSBE, Neal Viradia, MD, MPH. P0800 - Sinister Sequalae – A Rare Case of Left Sided Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
