Sunday Poster Session
Category: General Endoscopy
P0716 - The Peeling Puzzle: Understanding Esophagitis Dissecans Superficialis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Maitree Patel, MD, MBA
Palmetto General Hospital
Hialeah, FL
Presenting Author(s)
Maitree Patel, MD, MBA1, Aamir Saeed, MD2, Abdul Wasay, MD3, Srihita Patibandla, DO4, Roderick S. Brown, DO5
1Palmetto General Hospital, Hialeah, FL; 2Vanderbilt University Medical Center, Nashville, TN; 3University of Tennessee Medical Center, Knoxville, TN; 4Trinity Health Grand Rapids, Grand Rapids, MI; 5Hattiesburg GI Associates, Hattiesburg, MS
Introduction: Esophagitis dissecans superficialis (EDS), also known as sloughing esophagitis, is a rare condition characterized by superficial sloughing of the esophageal mucosa. Though less common than other esophagitis forms, EDS is increasingly recognized due to advancements in endoscopic imaging, and growing awareness. In esophagogastroduodenoscopy (EGD), it appears as stripped, whitish mucosa with or without bleeding, long linear mucosal breaks, and vertical cracks. EDS's causes are multifactorial, linked to GERD, eosinophilic esophagitis, medications like bisphosphonates or NSAIDs, chemical irritants, celiac disease, autoimmune bullous dermatoses, and idiopathic origins. This case report aims to contribute to the existing literature by presenting a unique case of EDS, detailing the patient's clinical history, diagnostic workup, and management, thereby enhancing the medical community's understanding of this distinctive esophageal entity.
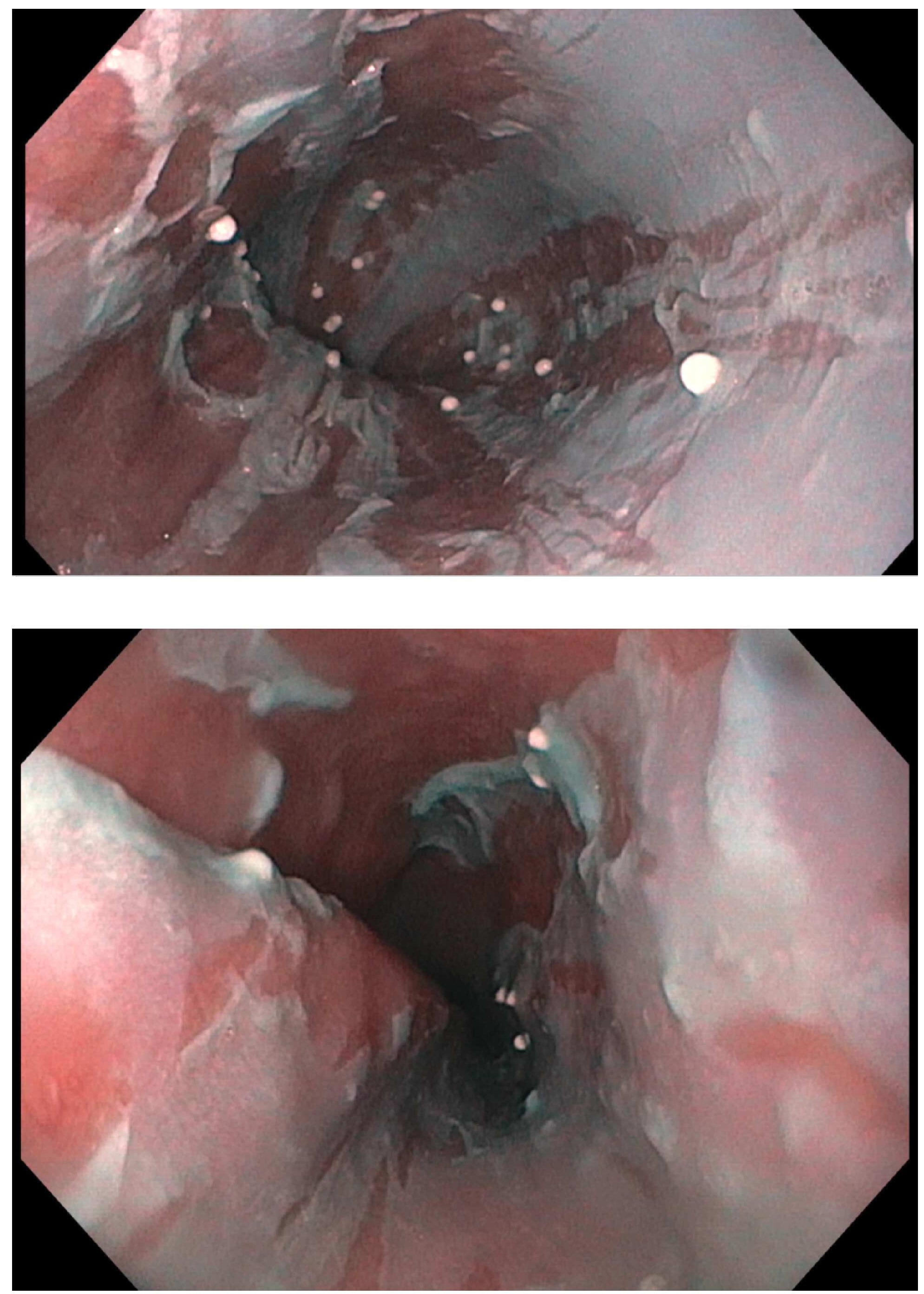
Case Description/Methods: A 77-year-old female presented with six months of dysphagia, describing solids getting stuck in her mid-chest. She had long-standing GERD and daily heartburn, managed with pantoprazole. She denied chest pain and shortness of breath. Her medical history included coronary artery disease, coronary artery bypass grafting, heart failure with preserved ejection fraction, and paroxysmal atrial fibrillation on Coumadin. An EGD assessed the cause of dysphagia. Linear areas of desquamative tissue were noted throughout the esophagus, consistent with EDS[Figure 1, 2, 3]. A cold forceps biopsy was obtained for histology. Dilation was deferred, pending biopsy results. The patient was treated by increasing pantoprazole to 80 mg daily. The dysphagia improved with treatment. No other association with EDS was identified.
Discussion: Recognizing EDS is crucial due to its potential to mimic other esophageal conditions, requiring a comprehensive diagnostic approach. Histological examination of biopsies is vital for confirming the diagnosis. EGD revealed characteristic linear areas of sloughed tissue, resembling EDS . Endoscopists must be aware of these findings to avoid confusion with esophagitis, squamous cell carcinoma, and infections. Further investigation is needed to confirm the diagnosis and determine the appropriate management plan. Management may include addressing GERD, optimizing therapy, and considering lifestyle changes.
Disclosures:
Maitree Patel, MD, MBA1, Aamir Saeed, MD2, Abdul Wasay, MD3, Srihita Patibandla, DO4, Roderick S. Brown, DO5. P0716 - The Peeling Puzzle: Understanding Esophagitis Dissecans Superficialis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Palmetto General Hospital, Hialeah, FL; 2Vanderbilt University Medical Center, Nashville, TN; 3University of Tennessee Medical Center, Knoxville, TN; 4Trinity Health Grand Rapids, Grand Rapids, MI; 5Hattiesburg GI Associates, Hattiesburg, MS
Introduction: Esophagitis dissecans superficialis (EDS), also known as sloughing esophagitis, is a rare condition characterized by superficial sloughing of the esophageal mucosa. Though less common than other esophagitis forms, EDS is increasingly recognized due to advancements in endoscopic imaging, and growing awareness. In esophagogastroduodenoscopy (EGD), it appears as stripped, whitish mucosa with or without bleeding, long linear mucosal breaks, and vertical cracks. EDS's causes are multifactorial, linked to GERD, eosinophilic esophagitis, medications like bisphosphonates or NSAIDs, chemical irritants, celiac disease, autoimmune bullous dermatoses, and idiopathic origins. This case report aims to contribute to the existing literature by presenting a unique case of EDS, detailing the patient's clinical history, diagnostic workup, and management, thereby enhancing the medical community's understanding of this distinctive esophageal entity.
Case Description/Methods: A 77-year-old female presented with six months of dysphagia, describing solids getting stuck in her mid-chest. She had long-standing GERD and daily heartburn, managed with pantoprazole. She denied chest pain and shortness of breath. Her medical history included coronary artery disease, coronary artery bypass grafting, heart failure with preserved ejection fraction, and paroxysmal atrial fibrillation on Coumadin. An EGD assessed the cause of dysphagia. Linear areas of desquamative tissue were noted throughout the esophagus, consistent with EDS[Figure 1, 2, 3]. A cold forceps biopsy was obtained for histology. Dilation was deferred, pending biopsy results. The patient was treated by increasing pantoprazole to 80 mg daily. The dysphagia improved with treatment. No other association with EDS was identified.
Discussion: Recognizing EDS is crucial due to its potential to mimic other esophageal conditions, requiring a comprehensive diagnostic approach. Histological examination of biopsies is vital for confirming the diagnosis. EGD revealed characteristic linear areas of sloughed tissue, resembling EDS . Endoscopists must be aware of these findings to avoid confusion with esophagitis, squamous cell carcinoma, and infections. Further investigation is needed to confirm the diagnosis and determine the appropriate management plan. Management may include addressing GERD, optimizing therapy, and considering lifestyle changes.
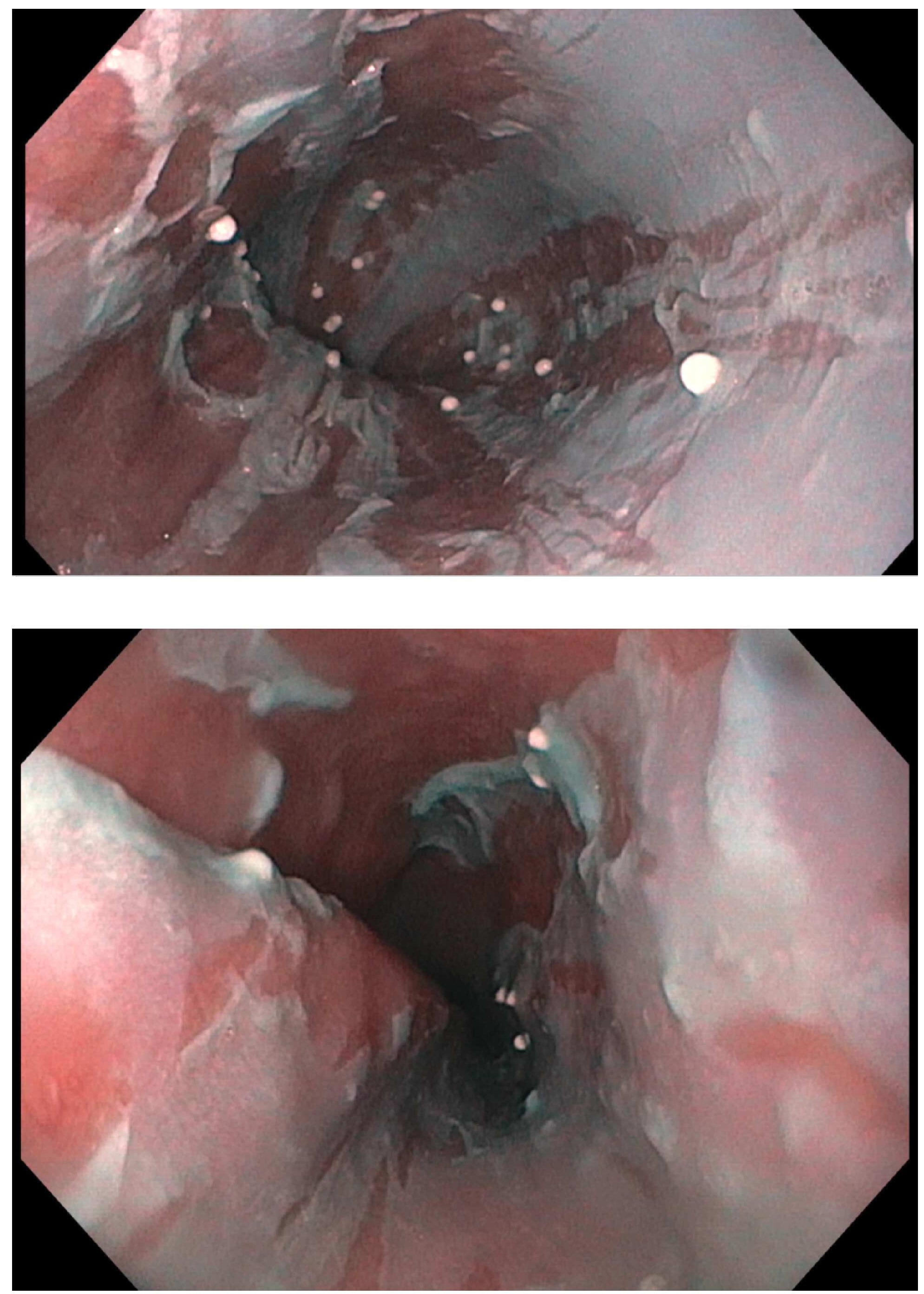
Figure: In EGD, stripped, whitish mucosa without bleeding, and long linear mucosal breaks(Linear areas of desquamative tissue) were noted throughout the esophagus, consistent with EDS.
Disclosures:
Maitree Patel indicated no relevant financial relationships.
Aamir Saeed indicated no relevant financial relationships.
Abdul Wasay indicated no relevant financial relationships.
Srihita Patibandla indicated no relevant financial relationships.
Roderick Brown indicated no relevant financial relationships.
Maitree Patel, MD, MBA1, Aamir Saeed, MD2, Abdul Wasay, MD3, Srihita Patibandla, DO4, Roderick S. Brown, DO5. P0716 - The Peeling Puzzle: Understanding Esophagitis Dissecans Superficialis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
