Sunday Poster Session
Category: General Endoscopy
P0723 - Management Challenges in Gardner’s Syndrome: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Jennifer Asotibe, MD
Montefiore Medical Center, Albert Einstein College of Medicine
New York, NY
Presenting Author(s)
Jennifer Asotibe, MD1, Fnu Vikash, MD, M.Med2, Donald P. Kotler, MD3
1Montefiore Medical Center, Albert Einstein College of Medicine, New York, NY; 2Albert Einstein College of Medicine, New York, NY; 3Jacobi Medical Center/North Central Bronx Hospital/Albert Einstein College of Medicine, Bronx, NY
Introduction: The management of Familial Adenomatous Polyposis (FAP) classically has been total proctocolectomy. However, there are variants of the disease which require modifications of therapy e.g. duodenal ampullary adenomas which have malignant potential and are best treated with a Whipple procedure. The condition may include coexisting tumors, notably desmoid tumors in which resection without damaging surrounding structures is difficult. Here we present a patient with this management dilemma.
Case Description/Methods: A 32-year-old male was admitted with abdominal discomfort and an abdominal mass for over a year, plus weight loss of 11 lbs over 9 months. The patient had been diagnosed with FAP and underwent subtotal colectomy in 2011 but was lost to follow up. He also was treated for epidermal inclusion cysts. Despite a few contacts with the health care system, he was not formally re-evaluated until the current admission
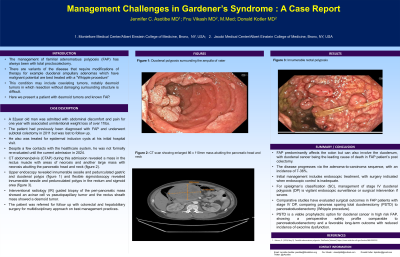
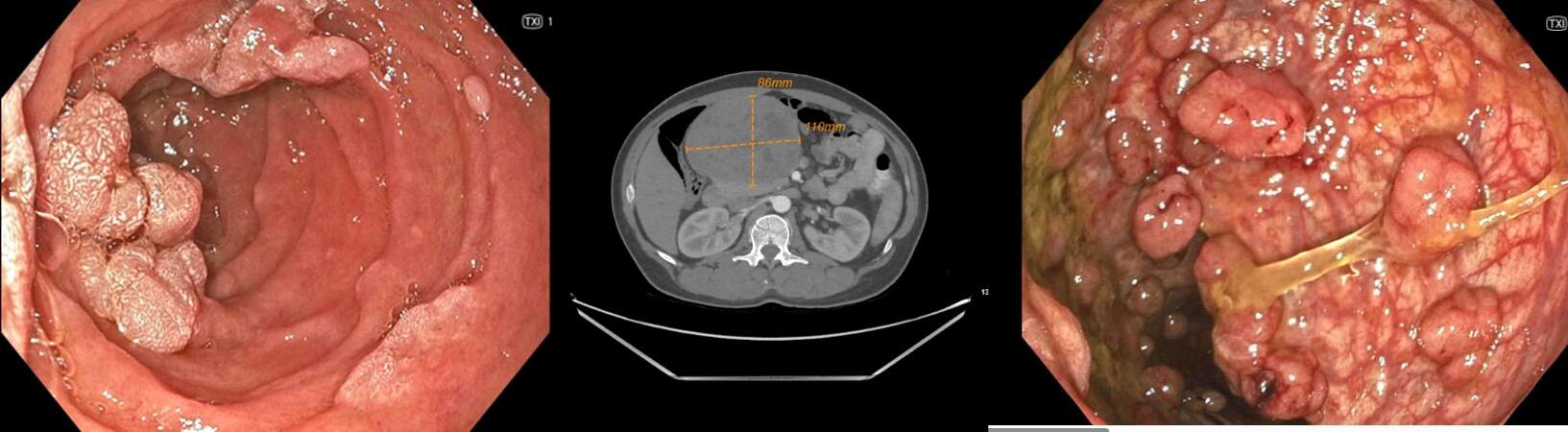
CTAP revealed a mass in the rectus muscle with areas of necrosis and another large mass with necrosis abutting the pancreatic head and neck (Fig 2). Upper endoscopy showed innumerable sessile and pedunculated gastric and duodenal polyps (Fig 1) and flexible sigmoidoscopy revealed innumerable sessile and pedunculated polyps in the rectum and sigmoid area (Fig 3). An IR-guided biopsy of the peripancreatic mass showed an acinar cell vs pseudopapillary tumor and the rectus sheath mass showed a desmoid tumor.
Discussion: Familial adenomatous polyposis (FAP) predominantly affects the colon but can also involve the duodenum, with duodenal cancer being the leading cause of death in FAP patients’ post-colectomy. The disease progresses via the adenoma-to-carcinoma sequence, with an incidence of 7-36%. Initial management includes endoscopic treatment, with surgery indicated when endoscopic control is inadequate. For Spigelman's Classification (SC) stage IV duodenal polyposis (DP), vigilant endoscopic surveillance or surgical intervention is required.
Comparative studies have evaluated surgical outcomes in FAP patients with SC stage IV DP, comparing pancreas-sparing total duodenectomy (PSTD) to pancreatoduodenectomy (Whipple procedure). PSTD is a viable prophylactic option for duodenal cancer in high-risk FAP, showing a perioperative safety profile comparable to pancreatoduodenectomy and a favorable long-term outcome with reduced incidence of exocrine dysfunction.
Disclosures:
Jennifer Asotibe, MD1, Fnu Vikash, MD, M.Med2, Donald P. Kotler, MD3. P0723 - Management Challenges in Gardner’s Syndrome: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Montefiore Medical Center, Albert Einstein College of Medicine, New York, NY; 2Albert Einstein College of Medicine, New York, NY; 3Jacobi Medical Center/North Central Bronx Hospital/Albert Einstein College of Medicine, Bronx, NY
Introduction: The management of Familial Adenomatous Polyposis (FAP) classically has been total proctocolectomy. However, there are variants of the disease which require modifications of therapy e.g. duodenal ampullary adenomas which have malignant potential and are best treated with a Whipple procedure. The condition may include coexisting tumors, notably desmoid tumors in which resection without damaging surrounding structures is difficult. Here we present a patient with this management dilemma.
Case Description/Methods: A 32-year-old male was admitted with abdominal discomfort and an abdominal mass for over a year, plus weight loss of 11 lbs over 9 months. The patient had been diagnosed with FAP and underwent subtotal colectomy in 2011 but was lost to follow up. He also was treated for epidermal inclusion cysts. Despite a few contacts with the health care system, he was not formally re-evaluated until the current admission
CTAP revealed a mass in the rectus muscle with areas of necrosis and another large mass with necrosis abutting the pancreatic head and neck (Fig 2). Upper endoscopy showed innumerable sessile and pedunculated gastric and duodenal polyps (Fig 1) and flexible sigmoidoscopy revealed innumerable sessile and pedunculated polyps in the rectum and sigmoid area (Fig 3). An IR-guided biopsy of the peripancreatic mass showed an acinar cell vs pseudopapillary tumor and the rectus sheath mass showed a desmoid tumor.
Discussion: Familial adenomatous polyposis (FAP) predominantly affects the colon but can also involve the duodenum, with duodenal cancer being the leading cause of death in FAP patients’ post-colectomy. The disease progresses via the adenoma-to-carcinoma sequence, with an incidence of 7-36%. Initial management includes endoscopic treatment, with surgery indicated when endoscopic control is inadequate. For Spigelman's Classification (SC) stage IV duodenal polyposis (DP), vigilant endoscopic surveillance or surgical intervention is required.
Comparative studies have evaluated surgical outcomes in FAP patients with SC stage IV DP, comparing pancreas-sparing total duodenectomy (PSTD) to pancreatoduodenectomy (Whipple procedure). PSTD is a viable prophylactic option for duodenal cancer in high-risk FAP, showing a perioperative safety profile comparable to pancreatoduodenectomy and a favorable long-term outcome with reduced incidence of exocrine dysfunction.
Figure: Figure 1: Duodenal polyposis surrounding the ampulla of water; Figure 2: CT scan showing enlarged 86 x 110mm mass abutting pancreatic head and neck; Figure 3: Innumerable rectal polyposis
Disclosures:
Jennifer Asotibe indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Donald P. Kotler: EMD Serono – Consultant.
Jennifer Asotibe, MD1, Fnu Vikash, MD, M.Med2, Donald P. Kotler, MD3. P0723 - Management Challenges in Gardner’s Syndrome: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
