Sunday Poster Session
Category: GI Bleeding
P0727 - Functional Disability After Clinically Significant Extracranial Bleeding: A Post Hoc ASPREE Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Darrick Li, MD, PhD
Yale School of Medicine / Connecticut GI
New London, CT
Presenting Author(s)
Darrick Li, MD, PhD1, David Cheng, PhD2, Anna Parks, MD3, Meghan Rieu-Warden, BS2, Galina Polekhina, PhD4, Suzanne Mahady, MD, PhD4, M. Maria Glymour, 5, Andrew Chan, MD, MPH6, Sachin Shah, MD, MPH6
1Yale School of Medicine / Connecticut GI, New London, CT; 2Massachusetts General Hospital, Boston, MA; 3University of Utah School of Medicine, Salt Lake City, UT; 4Monash University, Melbourne, Victoria, Australia; 5Boston University, Boston, MA; 6Massachusetts General Hospital, Harvard Medical School, Boston, MA
Introduction: Extracranial bleeding, including gastrointestinal (GI) bleeding, is a common side effect of antithrombotic agents. While short-term bleeding outcomes, including hospitalization and procedural intervention, are well-studied, the effect of extracranial bleeding on long-term outcomes, including functional independence, is poorly understood.
Methods: We conducted a secondary analysis of ASPREE, a randomized, placebo-controlled trial that tested the effect of low-dose aspirin on disability-free survival among healthy older adults. The primary outcome of this study was incident dependence in the Katz Activities of Daily Living (ADL), defined as being unable to perform any ADL independently or being admitted to a long-term care facility. We fit a multivariable Cox proportional hazard model for time to ADL dependence with occurrence of extracranial bleeding as a time-dependent covariate, adjusting for potential confounders. In secondary analyses, we assessed associations separately for patients with either GI or non-GI extracranial bleeds compared to patients without any bleeds. We also conducted stratified analysis of all extracranial bleeds by randomization arm (aspirin vs. placebo) by fitting an extended model that additionally included a main effect for randomization arm and an interaction between occurrence of extracranial bleeding and arm.
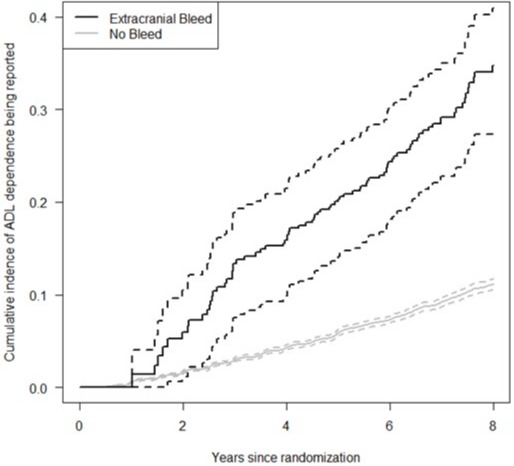
Results: Our study cohort included 18,982 participants followed for a median of 6.2 years, of whom 547 (2.9%) developed clinically significant extracranial bleeding (n=317 with GI bleeding). In multivariable-adjusted analysis, clinically significant extracranial bleeding was associated with incident ADL dependence (HR 2.46, 95% CI 1.97-3.07). The association of bleeding and incident ADL dependence was similar for extracranial bleeding from the GI tract (HR 2.30, 95% CI 1.72-3.08) and bleeding from non-GI causes (HR 2.68, 95% CI 1.95-3.69). Extracranial bleeding exhibited a weaker association with ADL dependence among patients randomized to aspirin (HR 2.15, 95% CI, 1.57-2.94) than among patients randomized to placebo (HR 2.84, 95% CI, 2.09-3.86), though the difference was not statistically significant (p-interaction=0.210).
Discussion: Clinically significant extracranial bleeding was associated with incident ADL dependence in otherwise healthy older adults. The potential impact of extracranial bleeding on long-term functional independence should be considered in risk/benefit discussions of antithrombotic agents.
Disclosures:
Darrick Li, MD, PhD1, David Cheng, PhD2, Anna Parks, MD3, Meghan Rieu-Warden, BS2, Galina Polekhina, PhD4, Suzanne Mahady, MD, PhD4, M. Maria Glymour, 5, Andrew Chan, MD, MPH6, Sachin Shah, MD, MPH6. P0727 - Functional Disability After Clinically Significant Extracranial Bleeding: A <i>Post Hoc</i> ASPREE Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale School of Medicine / Connecticut GI, New London, CT; 2Massachusetts General Hospital, Boston, MA; 3University of Utah School of Medicine, Salt Lake City, UT; 4Monash University, Melbourne, Victoria, Australia; 5Boston University, Boston, MA; 6Massachusetts General Hospital, Harvard Medical School, Boston, MA
Introduction: Extracranial bleeding, including gastrointestinal (GI) bleeding, is a common side effect of antithrombotic agents. While short-term bleeding outcomes, including hospitalization and procedural intervention, are well-studied, the effect of extracranial bleeding on long-term outcomes, including functional independence, is poorly understood.
Methods: We conducted a secondary analysis of ASPREE, a randomized, placebo-controlled trial that tested the effect of low-dose aspirin on disability-free survival among healthy older adults. The primary outcome of this study was incident dependence in the Katz Activities of Daily Living (ADL), defined as being unable to perform any ADL independently or being admitted to a long-term care facility. We fit a multivariable Cox proportional hazard model for time to ADL dependence with occurrence of extracranial bleeding as a time-dependent covariate, adjusting for potential confounders. In secondary analyses, we assessed associations separately for patients with either GI or non-GI extracranial bleeds compared to patients without any bleeds. We also conducted stratified analysis of all extracranial bleeds by randomization arm (aspirin vs. placebo) by fitting an extended model that additionally included a main effect for randomization arm and an interaction between occurrence of extracranial bleeding and arm.
Results: Our study cohort included 18,982 participants followed for a median of 6.2 years, of whom 547 (2.9%) developed clinically significant extracranial bleeding (n=317 with GI bleeding). In multivariable-adjusted analysis, clinically significant extracranial bleeding was associated with incident ADL dependence (HR 2.46, 95% CI 1.97-3.07). The association of bleeding and incident ADL dependence was similar for extracranial bleeding from the GI tract (HR 2.30, 95% CI 1.72-3.08) and bleeding from non-GI causes (HR 2.68, 95% CI 1.95-3.69). Extracranial bleeding exhibited a weaker association with ADL dependence among patients randomized to aspirin (HR 2.15, 95% CI, 1.57-2.94) than among patients randomized to placebo (HR 2.84, 95% CI, 2.09-3.86), though the difference was not statistically significant (p-interaction=0.210).
Discussion: Clinically significant extracranial bleeding was associated with incident ADL dependence in otherwise healthy older adults. The potential impact of extracranial bleeding on long-term functional independence should be considered in risk/benefit discussions of antithrombotic agents.
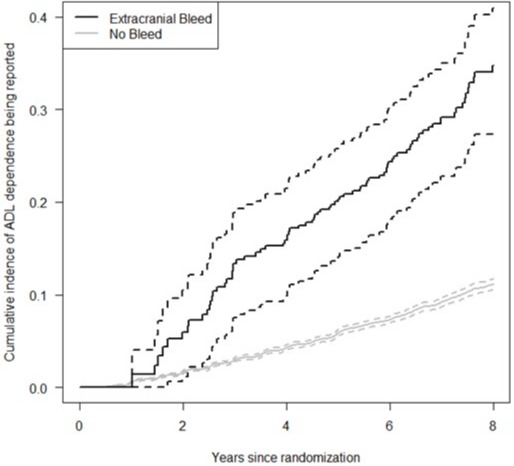
Figure: Unadjusted cumulative incidence of ADL dependence stratified by clinically significant extracranial bleeding
Disclosures:
Darrick Li: Phathom Pharmaceuticals – Speakers Bureau.
David Cheng indicated no relevant financial relationships.
Anna Parks indicated no relevant financial relationships.
Meghan Rieu-Warden indicated no relevant financial relationships.
Galina Polekhina indicated no relevant financial relationships.
Suzanne Mahady indicated no relevant financial relationships.
M. Maria Glymour indicated no relevant financial relationships.
Andrew Chan: Bayer Pharma AG – Consultant. Boehringer Ingelheim – Consultant. Pfizer – Consultant.
Sachin Shah indicated no relevant financial relationships.
Darrick Li, MD, PhD1, David Cheng, PhD2, Anna Parks, MD3, Meghan Rieu-Warden, BS2, Galina Polekhina, PhD4, Suzanne Mahady, MD, PhD4, M. Maria Glymour, 5, Andrew Chan, MD, MPH6, Sachin Shah, MD, MPH6. P0727 - Functional Disability After Clinically Significant Extracranial Bleeding: A <i>Post Hoc</i> ASPREE Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

