Sunday Poster Session
Category: Functional Bowel Disease
P0645 - Trends of Atrial Fibrillation Among Patients With Irritable Bowel Syndrome: A Five-Year Retrospective Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SP
Sreeram Pannala, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Alaukika Agarwal, MD1, Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Southern Illinois University, Springfield, IL
Introduction: Atrial fibrillation (AFib) and Irritable Bowel Syndrome (IBS) are distinct pathologies that affect different organ systems. However, emerging evidence suggests that dysbiosis frequently observed in IBS may lead to autonomic dysfunction and subsequent development of AFib. Our study aimed to investigate the development of AFib in patients diagnosed with IBS and compare the trends over five years.
Methods: We utilized the National Inpatient Sample (NIS) from 2016-2020 to identify patients affected by IBS using pertinent ICD-10 codes. We included all individuals with a primary or secondary diagnosis of IBS, above the age of 18. We outlined baseline characteristics using Pearson correlation and used regression analysis to analyze the risk of developing AFib. We adjusted for the odds of Afib by year of admission, gender & race.
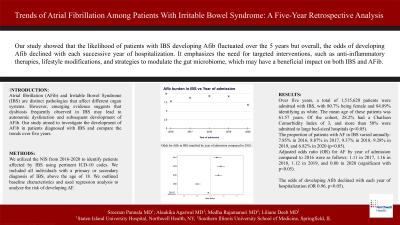
Results: Over five years, a total of 1,515,620 patients were admitted with IBS, with 80.7% being female and 84.89% identifying as White. The mean age of these patients was 61.57 years. Of the cohort, 28.2% had a Charlson Comorbidity Index of 3, and more than 50% were admitted to large bed-sized hospitals (p< 0.05).
The proportion of patients with Afib in IBS varied annually: 7.85% in 2016, 8.87% in 2017, 9.37% in 2018, 9.28% in 2019, and 6.82% in 2020 (p< 0.05). Over the five years, 9.19% of White patients with IBS had Afib, while approximately 5% of Blacks, Hispanics, and Asians had Afib (p< 0.05).
Adjusted odds (OR) for Afib by year of admission compared to 2016 were as follows: 1.11 in 2017, 1.16 in 2018, 1.12 in 2019, and 0.80 in 2020 (all p< 0.05). Adjusted for gender, females had lower odds of Afib (OR 0.69, p< 0.05). Stratified by race, compared to Whites; Blacks, Hispanics, and Asians had lower odds of Afib over five years (OR 0.79, 0.66, and 0.62, respectively; p< 0.05). Finally, the odds of developing Afib declined with each year of hospitalization (OR 0.96, p< 0.05).
Discussion: Our study showed that the likelihood of patients with IBS developing Afib fluctuated over the years but overall, the odds of developing Afib declined with each successive year of hospitalization. It emphasizes the need for targeted interventions, such as anti-inflammatory therapies, lifestyle modifications, and strategies to modulate the gut microbiome, which may have a beneficial impact on both IBS and AFib. Further research is needed to fully elucidate the mechanisms underlying the connection between IBS and AFib, paving the way for innovative approaches to prevention and treatment.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alaukika Agarwal, MD1, Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2. P0645 - Trends of Atrial Fibrillation Among Patients With Irritable Bowel Syndrome: A Five-Year Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Southern Illinois University, Springfield, IL
Introduction: Atrial fibrillation (AFib) and Irritable Bowel Syndrome (IBS) are distinct pathologies that affect different organ systems. However, emerging evidence suggests that dysbiosis frequently observed in IBS may lead to autonomic dysfunction and subsequent development of AFib. Our study aimed to investigate the development of AFib in patients diagnosed with IBS and compare the trends over five years.
Methods: We utilized the National Inpatient Sample (NIS) from 2016-2020 to identify patients affected by IBS using pertinent ICD-10 codes. We included all individuals with a primary or secondary diagnosis of IBS, above the age of 18. We outlined baseline characteristics using Pearson correlation and used regression analysis to analyze the risk of developing AFib. We adjusted for the odds of Afib by year of admission, gender & race.
Results: Over five years, a total of 1,515,620 patients were admitted with IBS, with 80.7% being female and 84.89% identifying as White. The mean age of these patients was 61.57 years. Of the cohort, 28.2% had a Charlson Comorbidity Index of 3, and more than 50% were admitted to large bed-sized hospitals (p< 0.05).
The proportion of patients with Afib in IBS varied annually: 7.85% in 2016, 8.87% in 2017, 9.37% in 2018, 9.28% in 2019, and 6.82% in 2020 (p< 0.05). Over the five years, 9.19% of White patients with IBS had Afib, while approximately 5% of Blacks, Hispanics, and Asians had Afib (p< 0.05).
Adjusted odds (OR) for Afib by year of admission compared to 2016 were as follows: 1.11 in 2017, 1.16 in 2018, 1.12 in 2019, and 0.80 in 2020 (all p< 0.05). Adjusted for gender, females had lower odds of Afib (OR 0.69, p< 0.05). Stratified by race, compared to Whites; Blacks, Hispanics, and Asians had lower odds of Afib over five years (OR 0.79, 0.66, and 0.62, respectively; p< 0.05). Finally, the odds of developing Afib declined with each year of hospitalization (OR 0.96, p< 0.05).
Discussion: Our study showed that the likelihood of patients with IBS developing Afib fluctuated over the years but overall, the odds of developing Afib declined with each successive year of hospitalization. It emphasizes the need for targeted interventions, such as anti-inflammatory therapies, lifestyle modifications, and strategies to modulate the gut microbiome, which may have a beneficial impact on both IBS and AFib. Further research is needed to fully elucidate the mechanisms underlying the connection between IBS and AFib, paving the way for innovative approaches to prevention and treatment.

Figure: Image illustrating the proportions of Afib in admitted patients with IBS over 5 years from 2016 to 2020.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alaukika Agarwal indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Medha Rajamanuri indicated no relevant financial relationships.
Alaukika Agarwal, MD1, Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2. P0645 - Trends of Atrial Fibrillation Among Patients With Irritable Bowel Syndrome: A Five-Year Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
