Sunday Poster Session
Category: Functional Bowel Disease
P0653 - Evidence of Altered Enteric Nervous System Structure Associated With Severe Dysmotility in a Patient With Ehlers-Danlos Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KO
Karina Oelerich, MD
Beth Israel Deaconess Medical Center
Boston, MA
Presenting Author(s)
Karina Oelerich, MD1, Scott B. Minchenberg, MD, PhD1, Kanwal Bains, MD2, Johanna Iturrino, MD3, Subhash Kulkarni, PhD1
1Beth Israel Deaconess Medical Center, Boston, MA; 2Banner - University of Arizona, Tucson, AZ; 3BIDMC, Chestnut Hill, MA
Introduction: Patients with Ehlers-Danlos Syndrome (EDS) often exhibit joint hypermobility, and suffer from gastroparesis, constipation, and whole gut dysmotility1. Since gut motility is regulated by cells of the enteric nervous system (ENS), it is widely assumed that gut dysmotility in EDS patients arises from pathologic alterations in the ENS tissue1,2. Due to the limitations of performing ENS-specific quantifiable pathological assessments on resected gut tissues, understanding ENS pathobiology is challenging. We present a case report of histopathological assessment of the ENS in resected gut tissue from an EDS patient with severe gut dysmotility.
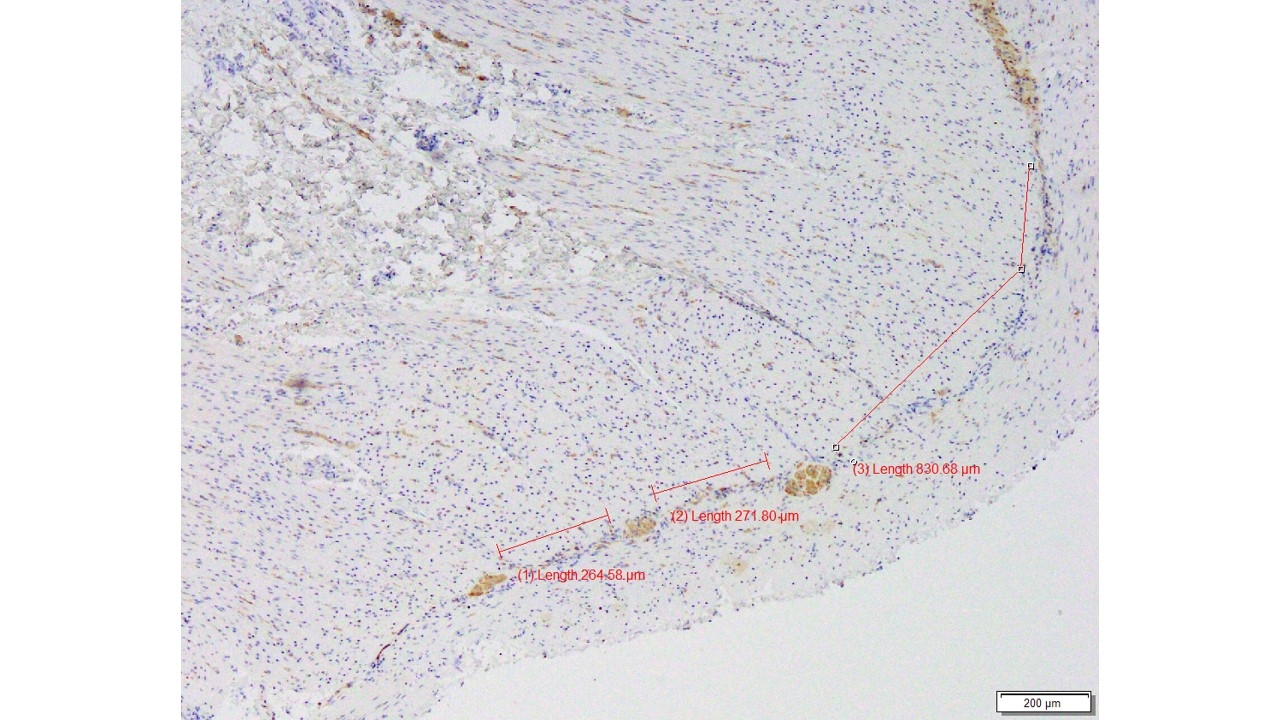
Case Description/Methods: A 26-year-old woman with a mutation in Fbn1 gene, history of EDS, gastroparesis, May-Thurners syndrome, sphincter of Oddi dysfunction and chronic mid-abdominal pain presented for evaluation of severe dysmotility - established by gastric emptying studies and anorectal manometry. Upper GI endoscopies had normal mucosal biopsy results; her course was complicated by multiple hospital admissions due to severe symptoms and infections. Numerous medications were tried with minimal benefit. Full thickness small bowel biopsy with immunostains for c-kit and S-100 within the myenteric plexus revealed no significant abnormality. We next used Boschetti et al.’s method2 of using Neuronal Specific Enolase (NSE)-based immunostaining to define normal vs abnormal ENS structure, and found that inter-ganglionic distance in the myenteric plexus of this patient (~800 um, Figure 1) exceeded the normal range for inter-ganglionic distance (380 - 570 um) established by Boschetti et al2. This histopathology fits the criteria for disordered ENS tissue associated with severe dysmotility.
Discussion: Evidence of disordered ENS has not been established in EDS patients due to the lack of application of existing quantitative metrics of ENS pathology, and lack of full thickness gut tissue. This case report highlights a pertinent point of using established metrics to identify structural abnormalities in EDS patient tissue. This clinical case provides strong rationale for pursuing histopathology in EDS patients, possibly through novel full thickness endoscopic resection methods.
1Alomari et al. Prevalence and Predictors of Gastrointestinal Dysmotility in Patients with Hypermobile Ehlers-Danlos Syndrome: A Tertiary Care Center Experience. 2020 Apr 29;12(4)
2Boschetti et al. Enteric neuron density correlates with clinical features of severe gut dysmotility. 2019 Dec 1;317(6).
Disclosures:
Karina Oelerich, MD1, Scott B. Minchenberg, MD, PhD1, Kanwal Bains, MD2, Johanna Iturrino, MD3, Subhash Kulkarni, PhD1. P0653 - Evidence of Altered Enteric Nervous System Structure Associated With Severe Dysmotility in a Patient With Ehlers-Danlos Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Boston, MA; 2Banner - University of Arizona, Tucson, AZ; 3BIDMC, Chestnut Hill, MA
Introduction: Patients with Ehlers-Danlos Syndrome (EDS) often exhibit joint hypermobility, and suffer from gastroparesis, constipation, and whole gut dysmotility1. Since gut motility is regulated by cells of the enteric nervous system (ENS), it is widely assumed that gut dysmotility in EDS patients arises from pathologic alterations in the ENS tissue1,2. Due to the limitations of performing ENS-specific quantifiable pathological assessments on resected gut tissues, understanding ENS pathobiology is challenging. We present a case report of histopathological assessment of the ENS in resected gut tissue from an EDS patient with severe gut dysmotility.
Case Description/Methods: A 26-year-old woman with a mutation in Fbn1 gene, history of EDS, gastroparesis, May-Thurners syndrome, sphincter of Oddi dysfunction and chronic mid-abdominal pain presented for evaluation of severe dysmotility - established by gastric emptying studies and anorectal manometry. Upper GI endoscopies had normal mucosal biopsy results; her course was complicated by multiple hospital admissions due to severe symptoms and infections. Numerous medications were tried with minimal benefit. Full thickness small bowel biopsy with immunostains for c-kit and S-100 within the myenteric plexus revealed no significant abnormality. We next used Boschetti et al.’s method2 of using Neuronal Specific Enolase (NSE)-based immunostaining to define normal vs abnormal ENS structure, and found that inter-ganglionic distance in the myenteric plexus of this patient (~800 um, Figure 1) exceeded the normal range for inter-ganglionic distance (380 - 570 um) established by Boschetti et al2. This histopathology fits the criteria for disordered ENS tissue associated with severe dysmotility.
Discussion: Evidence of disordered ENS has not been established in EDS patients due to the lack of application of existing quantitative metrics of ENS pathology, and lack of full thickness gut tissue. This case report highlights a pertinent point of using established metrics to identify structural abnormalities in EDS patient tissue. This clinical case provides strong rationale for pursuing histopathology in EDS patients, possibly through novel full thickness endoscopic resection methods.
1Alomari et al. Prevalence and Predictors of Gastrointestinal Dysmotility in Patients with Hypermobile Ehlers-Danlos Syndrome: A Tertiary Care Center Experience. 2020 Apr 29;12(4)
2Boschetti et al. Enteric neuron density correlates with clinical features of severe gut dysmotility. 2019 Dec 1;317(6).
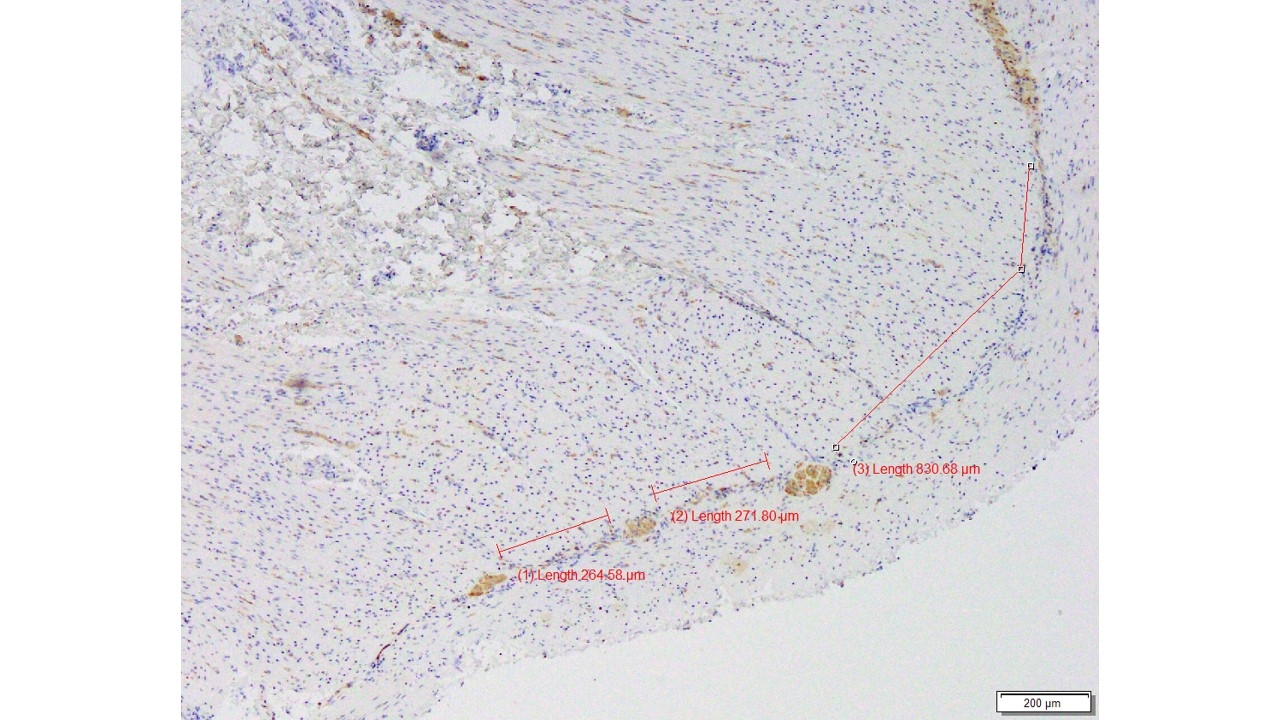
Figure: Image 1. Using immunostaining against NSE, we measured interganglionic distance in the ENS of an EDS patient
Disclosures:
Karina Oelerich indicated no relevant financial relationships.
Scott Minchenberg indicated no relevant financial relationships.
Kanwal Bains indicated no relevant financial relationships.
Johanna Iturrino indicated no relevant financial relationships.
Subhash Kulkarni indicated no relevant financial relationships.
Karina Oelerich, MD1, Scott B. Minchenberg, MD, PhD1, Kanwal Bains, MD2, Johanna Iturrino, MD3, Subhash Kulkarni, PhD1. P0653 - Evidence of Altered Enteric Nervous System Structure Associated With Severe Dysmotility in a Patient With Ehlers-Danlos Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
