Sunday Poster Session
Category: Esophagus
P0577 - Rare but Ruinous: Esophageal Epidermoid Metaplasia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Amanda Frondella, MD
UConn John Dempsey Hospital
Farmington, CT
Presenting Author(s)
Amanda Frondella, MD1, Rohit Singhania, MBBS, MS2
1UConn John Dempsey Hospital, Farmington, CT; 2Connecticut GI, Manchester, CT
Introduction: Esophageal epidermoid metaplasia (EEM), a rare finding on endoscopic biopsy, is a premalignant mucosal change that warrants prompt treatment because of its strong association with esophageal squamous cell carcinoma (ESCC). In this instance, we present a case of an EEM lesion treated with radiofrequency ablation (RFA) and subsequent monitoring.
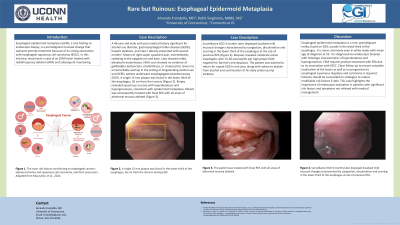
Case Description/Methods: A 46-year-old male with past medical history significant for alcohol use disorder, gastroesophageal reflux disease (GERD), hepatic steatosis, and Class I obesity presented with several months’ history of right upper quadrant pain, intermittently radiating to the epigastrium and back. Labs showed mildly elevated transaminases. HIDA scan showed no evidence of gallbladder dysfunction, cholelithiasis, or cholecystitis. Given his unremarkable workup in the setting of longstanding alcohol use and GERD, patient underwent esophagogastroduodenoscopy (EGD). A single 15 mm plaque was found in the lower third of the esophagus, 36 cm from the incisors (Figure 1a). Biopsy revealed squamous mucosa with hyperkeratosis and hypergranulosis, consistent with epidermoid metaplasia. Patient was consequently treated with focal RFA with all areas of abnormal mucosa ablated (Figure 1b).
Surveillance EGD 3 months later displayed localized mild mucosal changes characterized by congestion, discoloration and scarring in the lower third of the esophagus at the site of previous RFA (Figure 1c). Biopsies revealed moderate active esophagitis with 15-20 eosinophils per high power field: negative for Barrett’s and dysplasia. The patient was advised to return for repeat EGD in one year, along with advice to abstain from alcohol and continuation of his daily proton pump inhibitor.
Discussion: Esophageal epidermoid metaplasia is a rare, premalignant entity, found on EGD, usually in the distal third of the esophagus. It is more commonly seen in white males with mean age of diagnosis at 55. It is diagnosed via endoscopic biopsies with histologic characteristics of hyperkeratosis and hypergranulosis. EEM requires prompt treatment with RFA due to its association with ESCC. Close follow-up to ensure complete eradication of the lesion as well as no progression to esophageal squamous dysplasia and carcinoma is required. Patients should be counselled on strategies to reduce modifiable risk factors if able. This case highlights the importance of endoscopic evaluation in patients with significant risk factors and symptoms not relieved with medical management.

Disclosures:
Amanda Frondella, MD1, Rohit Singhania, MBBS, MS2. P0577 - Rare but Ruinous: Esophageal Epidermoid Metaplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UConn John Dempsey Hospital, Farmington, CT; 2Connecticut GI, Manchester, CT
Introduction: Esophageal epidermoid metaplasia (EEM), a rare finding on endoscopic biopsy, is a premalignant mucosal change that warrants prompt treatment because of its strong association with esophageal squamous cell carcinoma (ESCC). In this instance, we present a case of an EEM lesion treated with radiofrequency ablation (RFA) and subsequent monitoring.
Case Description/Methods: A 46-year-old male with past medical history significant for alcohol use disorder, gastroesophageal reflux disease (GERD), hepatic steatosis, and Class I obesity presented with several months’ history of right upper quadrant pain, intermittently radiating to the epigastrium and back. Labs showed mildly elevated transaminases. HIDA scan showed no evidence of gallbladder dysfunction, cholelithiasis, or cholecystitis. Given his unremarkable workup in the setting of longstanding alcohol use and GERD, patient underwent esophagogastroduodenoscopy (EGD). A single 15 mm plaque was found in the lower third of the esophagus, 36 cm from the incisors (Figure 1a). Biopsy revealed squamous mucosa with hyperkeratosis and hypergranulosis, consistent with epidermoid metaplasia. Patient was consequently treated with focal RFA with all areas of abnormal mucosa ablated (Figure 1b).
Surveillance EGD 3 months later displayed localized mild mucosal changes characterized by congestion, discoloration and scarring in the lower third of the esophagus at the site of previous RFA (Figure 1c). Biopsies revealed moderate active esophagitis with 15-20 eosinophils per high power field: negative for Barrett’s and dysplasia. The patient was advised to return for repeat EGD in one year, along with advice to abstain from alcohol and continuation of his daily proton pump inhibitor.
Discussion: Esophageal epidermoid metaplasia is a rare, premalignant entity, found on EGD, usually in the distal third of the esophagus. It is more commonly seen in white males with mean age of diagnosis at 55. It is diagnosed via endoscopic biopsies with histologic characteristics of hyperkeratosis and hypergranulosis. EEM requires prompt treatment with RFA due to its association with ESCC. Close follow-up to ensure complete eradication of the lesion as well as no progression to esophageal squamous dysplasia and carcinoma is required. Patients should be counselled on strategies to reduce modifiable risk factors if able. This case highlights the importance of endoscopic evaluation in patients with significant risk factors and symptoms not relieved with medical management.

Figure: Figure 1a) A single 15 mm plaque was found in the lower third of the esophagus, 36 cm from the incisors during EGD. b) The patient was treated with focal RFA with all areas of abnormal mucosa ablated. c) Surveillance EGD 3 months later displayed localized mild mucosal changes characterized by congestion, discoloration and scarring in the lower third of the esophagus at site of previous RFA.
Disclosures:
Amanda Frondella indicated no relevant financial relationships.
Rohit Singhania: Phathom pharmaceuticals – Speakers Bureau.
Amanda Frondella, MD1, Rohit Singhania, MBBS, MS2. P0577 - Rare but Ruinous: Esophageal Epidermoid Metaplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
