Sunday Poster Session
Category: Esophagus
P0578 - A Rare Cause of An Esophageal Respiratory Fistulae in a Patient With Dysphagia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Khalid Ahmed, MD
University of Pennsylvania
minneapolis, MN
Presenting Author(s)
Khalid Ahmed, MD1, Marwa Salman, MBBS2, Ayman Elawad, MD3, Elmkdad E. Mohammed, MD4
1University of Pennsylvania, Philadelphia, PA; 2University of Medical Sciences and Technology, Khartoum, Sudan, Philadelphia, PA; 3Massachusetts General Hospital, Boston, MA; 4The Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Esophageal respiratory fistulae are abnormal communications between the esophagus and the respiratory system. Acquired fistulae are usually secondary to infections or malignancy. Most of these fistulae are between the esophagus and trachea or bronchus, but abnormal connections between the esophagus and lung parenchyma are rare. We present a case of a 64-year-old male who was diagnosed with an esophago-parenchymal fistula secondary to stage III squamous cell carcinoma of the lung.
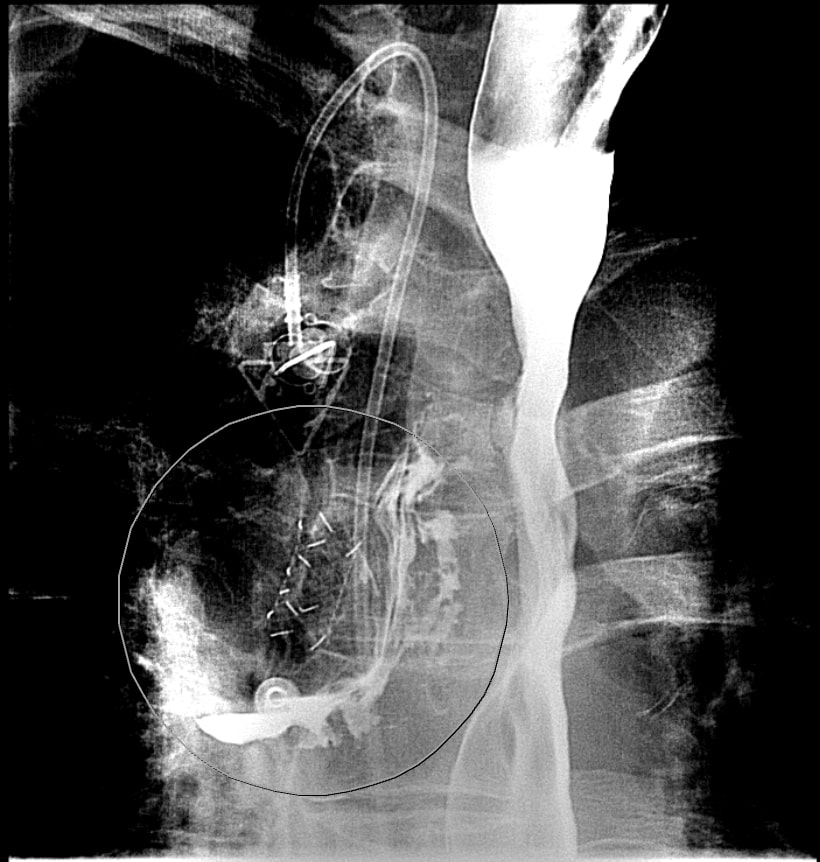
Case Description/Methods: 64-year-old male, with a past medical history of Squamous Cell Carcinoma of the lung status post chemoradiation and now on immunotherapy, chronic obstructive pulmonary disease and recurrent pneumonia who presented to the hospital after reportedly being found down at home. On presentation the patient had an altered mental status. He was hypotensive (91/60) and hypoxic requiring 3 liter via nasal cannula. Laboratory investigations were significant for leukocytosis and an elevated lactate. CT scan of the lung with contrast showed interval worsening of known lung mass with increased necrosis and cavitation of the mass. The patient was started on intravenous antibiotics and fluids. He was admitted for management of sepsis secondary to pneumonia. He improved clinically and responded appropriately to the management plan. The hospital course was complicated by reduced oral intake and dysphagia. He underwent a barium esophagogram which showed a malignant fistula between the upper esophagus and cavitary right upper lobe mass (figure 1). He underwent palliative placement of an endoluminal esophageal stent to occlude the fistula by fiberoptic esophagogastroduodenoscopy. The patient tolerated the procedure well. Follow up barium esophagogram showed interval placement of esophageal stent without evidence of leak. The diet was advanced accordingly, but with restrictions to avoid risks for stent occlusion.
Discussion: Esophageal-parenchymal fistulae must be suspected in patients with lung cancer who complain of dysphagia, especially with a history of recurrent pneumonia. Esophageal-parenchymal fistulae are diagnosed by radiological imaging, in our case a barium study. Because esophageal-parenchymal fistulae are a debilitating condition, prompt treatment with esophageal stenting is important in patients who are not surgical candidates. Early diagnosis and management can improve quality of life. No official guidelines exist, therefore more studies are needed to establish a comprehensive understanding.
Disclosures:
Khalid Ahmed, MD1, Marwa Salman, MBBS2, Ayman Elawad, MD3, Elmkdad E. Mohammed, MD4. P0578 - A Rare Cause of An Esophageal Respiratory Fistulae in a Patient With Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Pennsylvania, Philadelphia, PA; 2University of Medical Sciences and Technology, Khartoum, Sudan, Philadelphia, PA; 3Massachusetts General Hospital, Boston, MA; 4The Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Esophageal respiratory fistulae are abnormal communications between the esophagus and the respiratory system. Acquired fistulae are usually secondary to infections or malignancy. Most of these fistulae are between the esophagus and trachea or bronchus, but abnormal connections between the esophagus and lung parenchyma are rare. We present a case of a 64-year-old male who was diagnosed with an esophago-parenchymal fistula secondary to stage III squamous cell carcinoma of the lung.
Case Description/Methods: 64-year-old male, with a past medical history of Squamous Cell Carcinoma of the lung status post chemoradiation and now on immunotherapy, chronic obstructive pulmonary disease and recurrent pneumonia who presented to the hospital after reportedly being found down at home. On presentation the patient had an altered mental status. He was hypotensive (91/60) and hypoxic requiring 3 liter via nasal cannula. Laboratory investigations were significant for leukocytosis and an elevated lactate. CT scan of the lung with contrast showed interval worsening of known lung mass with increased necrosis and cavitation of the mass. The patient was started on intravenous antibiotics and fluids. He was admitted for management of sepsis secondary to pneumonia. He improved clinically and responded appropriately to the management plan. The hospital course was complicated by reduced oral intake and dysphagia. He underwent a barium esophagogram which showed a malignant fistula between the upper esophagus and cavitary right upper lobe mass (figure 1). He underwent palliative placement of an endoluminal esophageal stent to occlude the fistula by fiberoptic esophagogastroduodenoscopy. The patient tolerated the procedure well. Follow up barium esophagogram showed interval placement of esophageal stent without evidence of leak. The diet was advanced accordingly, but with restrictions to avoid risks for stent occlusion.
Discussion: Esophageal-parenchymal fistulae must be suspected in patients with lung cancer who complain of dysphagia, especially with a history of recurrent pneumonia. Esophageal-parenchymal fistulae are diagnosed by radiological imaging, in our case a barium study. Because esophageal-parenchymal fistulae are a debilitating condition, prompt treatment with esophageal stenting is important in patients who are not surgical candidates. Early diagnosis and management can improve quality of life. No official guidelines exist, therefore more studies are needed to establish a comprehensive understanding.
Figure: Figure 1. Barium study showing malignant esophago-parenchymal fistula
Disclosures:
Khalid Ahmed indicated no relevant financial relationships.
Marwa Salman indicated no relevant financial relationships.
Ayman Elawad indicated no relevant financial relationships.
Elmkdad Mohammed indicated no relevant financial relationships.
Khalid Ahmed, MD1, Marwa Salman, MBBS2, Ayman Elawad, MD3, Elmkdad E. Mohammed, MD4. P0578 - A Rare Cause of An Esophageal Respiratory Fistulae in a Patient With Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
