Sunday Poster Session
Category: Esophagus
P0583 - Lymphocytic Esophagitis Presenting in a Lichenoid Pattern
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KT
Kimberly Tena Diaz, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Kimberly Tena Diaz, DO1, Kathy N. Williams, MD, MS2, Tara Lautenslager, MD3, Tommy Nguyen, DO2
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Philadelphia, PA; 3Cooper Health Gastroenterology, Mount Laurel, NJ
Introduction: Lymphocytic esophagitis is a rare subtype of esophagitis established in 2006 by Rubio et al. after finding patients with a predominance of lymphocytes and few or no granulocytes. Lymphocytic esophagitis with a lichenoid pattern is particularly unique as there are few studies delineating this condition. Its distinction from lichen planus must be made as the presentation varies and treatment options differ.
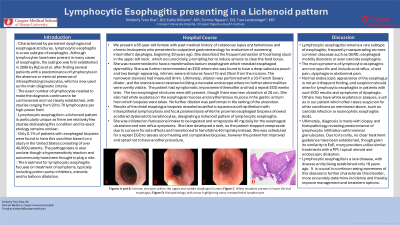
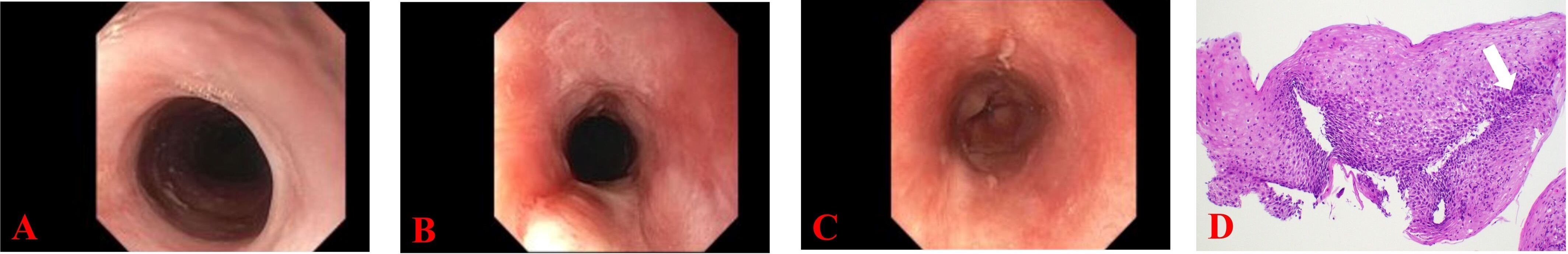
Case Description/Methods: We present a 65-year-old female with a past medical history of cutaneous lupus erythematosus who presented for evaluation of intermittent dysphagia of 30 years. She described daily episodes of globus sensation, prompting her to self-induce emesis. A barium esophagram demonstrated slowed clearance of food boluses. An EGD showed a deep vallecula pouch and two benign-appearing, severe strictures. A 33-Fr Savary dilator was used with mild resistance and the stenoses were traversed with a neonatal endoscope where no further abnormalities were overtly visible. The patient had symptomatic improvement thereafter. Repeat EGD two weeks later showed the same two esophageal strictures with a new esophageal ulceration. She also had white speckled mucosa in the esophagus and erythematous mucosa in the gastric antrum from which biopsies were taken. No further dilation was done in the setting of this ulceration. Results of the esophageal biopsies showed intraepithelial lymphocytosis, focal parakeratosis and scattered dyskeratotic keratinocytes, designating a lichenoid pattern of lymphocytic esophagitis. She was initiated on fluticasone inhaler to be ingested as well as omeprazole 40 mg daily. She was scheduled for a repeat EGD several months later, although the patient felt improved and opted not to have another procedure.
Discussion: Lymphocytic esophagitis is a rare subtype of esophagitis and suspicion of lymphocytic esophagitis should arise even in patients with dysphagia, but a normal EGD. Findings may include white exudates or plaques, which can be seen in other conditions such as lichen planus or eosinophilic esophagitis. Histopathology, however, will show predominance of lymphocytic infiltration with minimal granulocytes and no evidence of the typical Civatte bodies nor eosinophil predominance as seen in lichen planus and eosinophilic esophagitis. Due to its rarity, no clear treatment guidelines have been established, though many providers have extrapolated from other esophagitis treatments and utilize PPI, topical steroids and endoscopic dilatation as treatment options.
Disclosures:
Kimberly Tena Diaz, DO1, Kathy N. Williams, MD, MS2, Tara Lautenslager, MD3, Tommy Nguyen, DO2. P0583 - Lymphocytic Esophagitis Presenting in a Lichenoid Pattern, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Philadelphia, PA; 3Cooper Health Gastroenterology, Mount Laurel, NJ
Introduction: Lymphocytic esophagitis is a rare subtype of esophagitis established in 2006 by Rubio et al. after finding patients with a predominance of lymphocytes and few or no granulocytes. Lymphocytic esophagitis with a lichenoid pattern is particularly unique as there are few studies delineating this condition. Its distinction from lichen planus must be made as the presentation varies and treatment options differ.
Case Description/Methods: We present a 65-year-old female with a past medical history of cutaneous lupus erythematosus who presented for evaluation of intermittent dysphagia of 30 years. She described daily episodes of globus sensation, prompting her to self-induce emesis. A barium esophagram demonstrated slowed clearance of food boluses. An EGD showed a deep vallecula pouch and two benign-appearing, severe strictures. A 33-Fr Savary dilator was used with mild resistance and the stenoses were traversed with a neonatal endoscope where no further abnormalities were overtly visible. The patient had symptomatic improvement thereafter. Repeat EGD two weeks later showed the same two esophageal strictures with a new esophageal ulceration. She also had white speckled mucosa in the esophagus and erythematous mucosa in the gastric antrum from which biopsies were taken. No further dilation was done in the setting of this ulceration. Results of the esophageal biopsies showed intraepithelial lymphocytosis, focal parakeratosis and scattered dyskeratotic keratinocytes, designating a lichenoid pattern of lymphocytic esophagitis. She was initiated on fluticasone inhaler to be ingested as well as omeprazole 40 mg daily. She was scheduled for a repeat EGD several months later, although the patient felt improved and opted not to have another procedure.
Discussion: Lymphocytic esophagitis is a rare subtype of esophagitis and suspicion of lymphocytic esophagitis should arise even in patients with dysphagia, but a normal EGD. Findings may include white exudates or plaques, which can be seen in other conditions such as lichen planus or eosinophilic esophagitis. Histopathology, however, will show predominance of lymphocytic infiltration with minimal granulocytes and no evidence of the typical Civatte bodies nor eosinophil predominance as seen in lichen planus and eosinophilic esophagitis. Due to its rarity, no clear treatment guidelines have been established, though many providers have extrapolated from other esophagitis treatments and utilize PPI, topical steroids and endoscopic dilatation as treatment options.
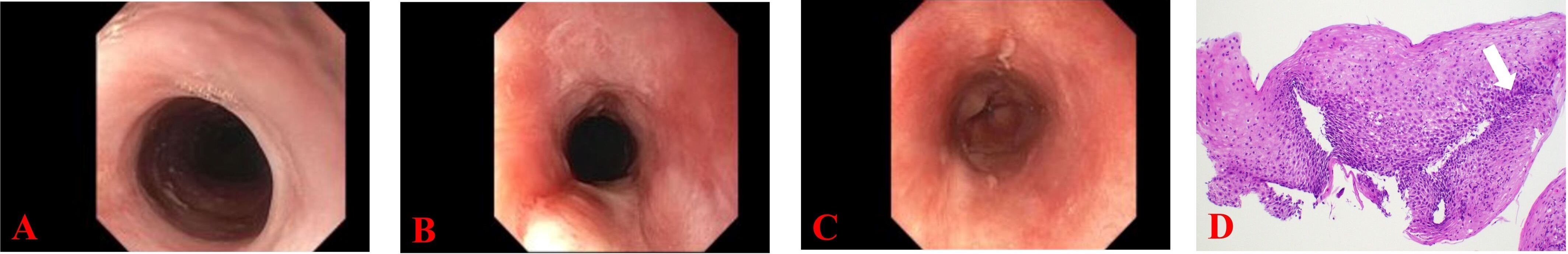
Figure: Figures A and B: Intrinsic strictures within the upper and middle esophageal lumen
Figure C: White exudates present in lower third of esophagus
Figure D: Histopathology with arrow highlighting many intraepithelial lymphocytes
Figure C: White exudates present in lower third of esophagus
Figure D: Histopathology with arrow highlighting many intraepithelial lymphocytes
Disclosures:
Kimberly Tena Diaz indicated no relevant financial relationships.
Kathy Williams indicated no relevant financial relationships.
Tara Lautenslager indicated no relevant financial relationships.
Tommy Nguyen indicated no relevant financial relationships.
Kimberly Tena Diaz, DO1, Kathy N. Williams, MD, MS2, Tara Lautenslager, MD3, Tommy Nguyen, DO2. P0583 - Lymphocytic Esophagitis Presenting in a Lichenoid Pattern, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
