Sunday Poster Session
Category: Esophagus
P0587 - Isolated Esophageal Vasculitis: An Atypical Presentation of Chest Pain
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Francisco M. Pascual, MD
University of South Florida Health
Tampa, FL
Presenting Author(s)
Francisco M. Pascual, MD1, Andres Cordoba, DO2, Ruha Reddy, BS3, Patrick Malafronte, MD4, Shreya Narayanan, MD2
1University of South Florida Health, Tampa, FL; 2University of South Florida, Tampa, FL; 3University of South Florida Morsani College of Medicine, Tampa, FL; 4Ruffolo, Hooper and Associates, Tampa, FL
Introduction: Gastrointestinal (GI) manifestations can be seen in various vasculitides; however, vasculitis restricted to the GI tract is rare, with limited supporting data. In the following case, we discuss a unique presentation of chest pain leading to the discovery of esophageal vasculitis without previously diagnosed systemic disease.
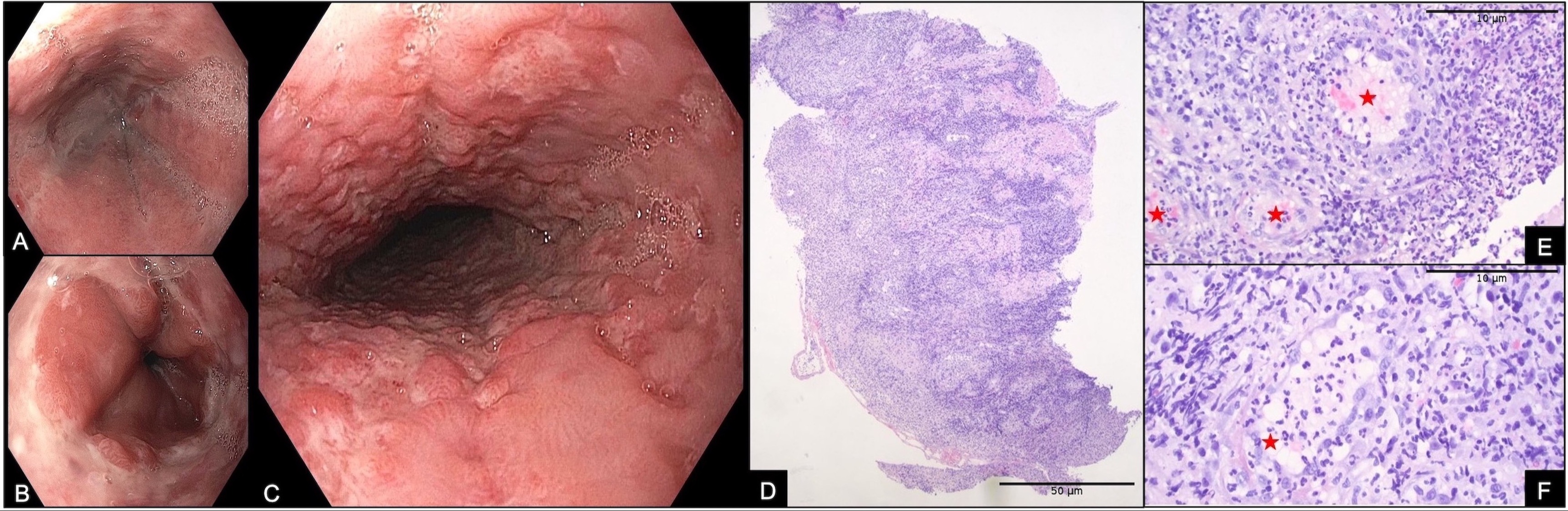
Case Description/Methods: A 42-year-old male with a past medical history of premature ischemic cardiomyopathy with reduced ejection fraction on dual antiplatelet therapy presented to the hospital with one week of episodic, centralized, crushing, post-prandial chest pain. The pain lasted 3-5 minutes and improved with passive leg raise. On admission, vital signs were within normal limits, physical exam was unremarkable, and laboratory studies revealed only a decreased hemoglobin of 12.2 g/dL from a baseline of 14 g/dL. Initial cardiac workup with EKG, serial troponins, and echocardiogram was unremarkable. Gastroenterology was consulted, and the patient underwent esophagogastroduodenoscopy, which revealed diffuse innumerable small cratered, non-bleeding esophageal ulcers with diffuse surrounding erythema and edema, with relative sparing of the distal esophagus. Biopsies were obtained, and histopathological analysis demonstrated ulcerated squamous mucosa and marked subepithelial acute and chronic inflammation, including dense inflammatory infiltrate, vascular damage, and vessels with fibrinoid mural necrosis. Granular C3 deposition in sub-epithelial blood vessels was noted on immunofluorescence. Sampling in Michel’s solution was negative for lichen planus. Based on these findings suggestive of vasculitis, the patient was referred to rheumatology for further workup.
Discussion: Given the limited data in the literature, the true incidence and prevalence of vasculitides isolated to the GI tract are difficult to quantify. Patients may present with a variety of GI symptoms or be asymptomatic entirely. Often, diagnosis is made incidentally, with the gallbladder being a common disease site identified post-cholecystectomy. This case highlights an essential aspect of GI vasculitis, as diagnosis largely relies on imaging or pathological findings. Routine surveillance following the identification of vasculitis isolated to the GI tract is vital as systemic vasculitis can develop in upwards of 25% of patients. In this case, the patient’s identified vasculitis may be a contributing factor to his premature coronary artery disease and sequelae.
Disclosures:
Francisco M. Pascual, MD1, Andres Cordoba, DO2, Ruha Reddy, BS3, Patrick Malafronte, MD4, Shreya Narayanan, MD2. P0587 - Isolated Esophageal Vasculitis: An Atypical Presentation of Chest Pain, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Health, Tampa, FL; 2University of South Florida, Tampa, FL; 3University of South Florida Morsani College of Medicine, Tampa, FL; 4Ruffolo, Hooper and Associates, Tampa, FL
Introduction: Gastrointestinal (GI) manifestations can be seen in various vasculitides; however, vasculitis restricted to the GI tract is rare, with limited supporting data. In the following case, we discuss a unique presentation of chest pain leading to the discovery of esophageal vasculitis without previously diagnosed systemic disease.
Case Description/Methods: A 42-year-old male with a past medical history of premature ischemic cardiomyopathy with reduced ejection fraction on dual antiplatelet therapy presented to the hospital with one week of episodic, centralized, crushing, post-prandial chest pain. The pain lasted 3-5 minutes and improved with passive leg raise. On admission, vital signs were within normal limits, physical exam was unremarkable, and laboratory studies revealed only a decreased hemoglobin of 12.2 g/dL from a baseline of 14 g/dL. Initial cardiac workup with EKG, serial troponins, and echocardiogram was unremarkable. Gastroenterology was consulted, and the patient underwent esophagogastroduodenoscopy, which revealed diffuse innumerable small cratered, non-bleeding esophageal ulcers with diffuse surrounding erythema and edema, with relative sparing of the distal esophagus. Biopsies were obtained, and histopathological analysis demonstrated ulcerated squamous mucosa and marked subepithelial acute and chronic inflammation, including dense inflammatory infiltrate, vascular damage, and vessels with fibrinoid mural necrosis. Granular C3 deposition in sub-epithelial blood vessels was noted on immunofluorescence. Sampling in Michel’s solution was negative for lichen planus. Based on these findings suggestive of vasculitis, the patient was referred to rheumatology for further workup.
Discussion: Given the limited data in the literature, the true incidence and prevalence of vasculitides isolated to the GI tract are difficult to quantify. Patients may present with a variety of GI symptoms or be asymptomatic entirely. Often, diagnosis is made incidentally, with the gallbladder being a common disease site identified post-cholecystectomy. This case highlights an essential aspect of GI vasculitis, as diagnosis largely relies on imaging or pathological findings. Routine surveillance following the identification of vasculitis isolated to the GI tract is vital as systemic vasculitis can develop in upwards of 25% of patients. In this case, the patient’s identified vasculitis may be a contributing factor to his premature coronary artery disease and sequelae.
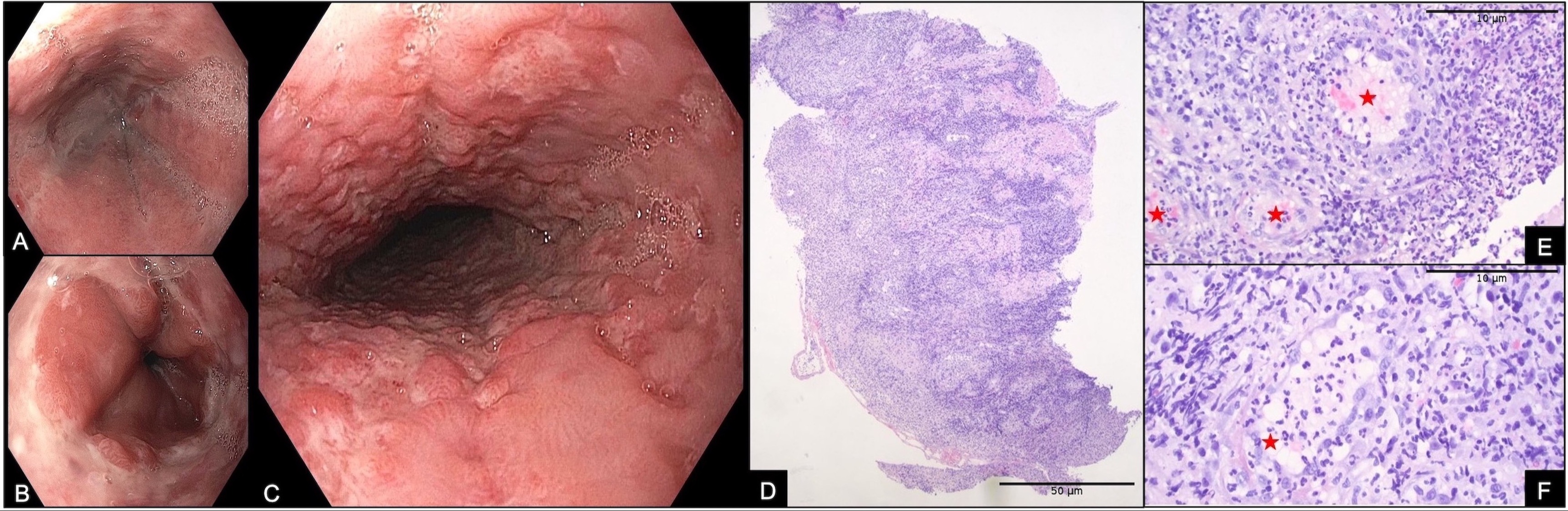
Figure: Figure 1.
A. Proximal esophagus.
B. Esophagogastric junction.
C. Mid esophagus.
D. Low-power photomicrograph of esophageal biopsy demonstrating surface ulceration on left and marked underlying subepithelial inflammatory infiltrate (H&E stain, 40X magnification, scale bar 50 µm).
E-F. High-power magnification demonstrating abundant background neutrophilic and lymphoplasmacytic inflammation with numerous vessels (red star) demonstrating mural neutrophils and light pink fibrinoid material (H&E stain, 200x magnification, scale bar 10 µm).
A. Proximal esophagus.
B. Esophagogastric junction.
C. Mid esophagus.
D. Low-power photomicrograph of esophageal biopsy demonstrating surface ulceration on left and marked underlying subepithelial inflammatory infiltrate (H&E stain, 40X magnification, scale bar 50 µm).
E-F. High-power magnification demonstrating abundant background neutrophilic and lymphoplasmacytic inflammation with numerous vessels (red star) demonstrating mural neutrophils and light pink fibrinoid material (H&E stain, 200x magnification, scale bar 10 µm).
Disclosures:
Francisco Pascual indicated no relevant financial relationships.
Andres Cordoba indicated no relevant financial relationships.
Ruha Reddy indicated no relevant financial relationships.
Patrick Malafronte indicated no relevant financial relationships.
Shreya Narayanan indicated no relevant financial relationships.
Francisco M. Pascual, MD1, Andres Cordoba, DO2, Ruha Reddy, BS3, Patrick Malafronte, MD4, Shreya Narayanan, MD2. P0587 - Isolated Esophageal Vasculitis: An Atypical Presentation of Chest Pain, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

