Sunday Poster Session
Category: Esophagus
P0593 - Underlying Eosinophilic Esophagitis Masquerading as an Upper GI Bleed
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Neil Gambhir, DO
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Neil Gambhir, DO1, Samantha Rubin, DO1, Noah Y. Mahpour, MD1, Arun Swaminath, MD2
1Lenox Hill Hospital, Northwell Health, New York, NY; 2Lenox Hill Hospital/Northwell Health, New York, NY
Introduction: Eosinophilic esophagitis (EoE) is an increasingly recognized autoimmune disorder characterized by eosinophilic infiltration of the esophagus. Diagnosis of EoE necessitates endoscopic evidence of abnormal esophageal changes with > 15 eosinophils per high power field (HPF) and patients typically endorse a history laden with dysphagic episodes. Herein, we describe the case of an adult male whose initial presentation was an upper GI bleed resulting from a Mallory Weiss tear, but ultimately was found to have underlying EoE.
Case Description/Methods: A 53-year-old male with a past medical history of a duodenal ulcer presented to our emergency room reporting several episodes of coffee ground emesis and melenic stools. These symptoms began after an episode of forceful retching after eating a cheesesteak sandwich with a described sensation of it becoming stuck in his chest. The patient endorsed that he had a similar sensation of food being stuck in his chest a week prior to admission, as well as a history of food sensitivities beginning in childhood. However, this sensation of food being stuck had not occurred prior to these two episodes.
The patient denied any abdominal pain at the time of presentation and vitals were significant for tachycardia to 142 beats per minute. Lab work was significant for a BUN of 29, Total bilirubin of 2.1, AST/ALT of 88/146 and Eosinophilia of 10.1%. His hemoglobin was 11.2mg/dL on admission.
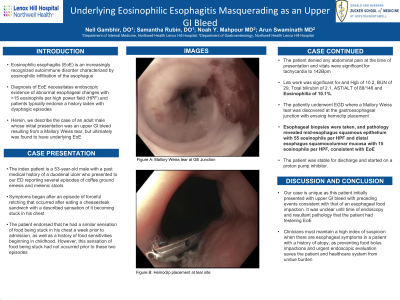
The patiently underwent upper endoscopy, where a benign esophageal stricture was encountered and subsequently traversed with minimal pressure. A Mallory Weiss tear was discovered at the gastroesophageal junction with ensuring hemoclip placement. Esophageal biopsies were taken, and pathology revealed mid-esophagus squamous epithelium with 55 eosinophils per high power field and distal esophagus squamocolumnar mucosa with 15 eosinophils per HPF, consistent with EoE. The patient was stable for discharge and started on a proton pump inhibitor.
Discussion: Our case is unique as this patient initially presented with upper GI bleed with preceding events consistent with that of an esophageal food impaction with subsequent retching. It was unclear until time of endoscopy and resultant pathology that the patient had festering EoE. Clinicians must maintain a high index of suspicion when there are esophageal symptoms in a patient with a history of atopy, as preventing food bolus impactions and urgent endoscopic evaluation saves the patient and healthcare system an undue burden.

Disclosures:
Neil Gambhir, DO1, Samantha Rubin, DO1, Noah Y. Mahpour, MD1, Arun Swaminath, MD2. P0593 - Underlying Eosinophilic Esophagitis Masquerading as an Upper GI Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lenox Hill Hospital, Northwell Health, New York, NY; 2Lenox Hill Hospital/Northwell Health, New York, NY
Introduction: Eosinophilic esophagitis (EoE) is an increasingly recognized autoimmune disorder characterized by eosinophilic infiltration of the esophagus. Diagnosis of EoE necessitates endoscopic evidence of abnormal esophageal changes with > 15 eosinophils per high power field (HPF) and patients typically endorse a history laden with dysphagic episodes. Herein, we describe the case of an adult male whose initial presentation was an upper GI bleed resulting from a Mallory Weiss tear, but ultimately was found to have underlying EoE.
Case Description/Methods: A 53-year-old male with a past medical history of a duodenal ulcer presented to our emergency room reporting several episodes of coffee ground emesis and melenic stools. These symptoms began after an episode of forceful retching after eating a cheesesteak sandwich with a described sensation of it becoming stuck in his chest. The patient endorsed that he had a similar sensation of food being stuck in his chest a week prior to admission, as well as a history of food sensitivities beginning in childhood. However, this sensation of food being stuck had not occurred prior to these two episodes.
The patient denied any abdominal pain at the time of presentation and vitals were significant for tachycardia to 142 beats per minute. Lab work was significant for a BUN of 29, Total bilirubin of 2.1, AST/ALT of 88/146 and Eosinophilia of 10.1%. His hemoglobin was 11.2mg/dL on admission.
The patiently underwent upper endoscopy, where a benign esophageal stricture was encountered and subsequently traversed with minimal pressure. A Mallory Weiss tear was discovered at the gastroesophageal junction with ensuring hemoclip placement. Esophageal biopsies were taken, and pathology revealed mid-esophagus squamous epithelium with 55 eosinophils per high power field and distal esophagus squamocolumnar mucosa with 15 eosinophils per HPF, consistent with EoE. The patient was stable for discharge and started on a proton pump inhibitor.
Discussion: Our case is unique as this patient initially presented with upper GI bleed with preceding events consistent with that of an esophageal food impaction with subsequent retching. It was unclear until time of endoscopy and resultant pathology that the patient had festering EoE. Clinicians must maintain a high index of suspicion when there are esophageal symptoms in a patient with a history of atopy, as preventing food bolus impactions and urgent endoscopic evaluation saves the patient and healthcare system an undue burden.

Figure: Mallory Weiss Tear Visualized on EGD with overlying blood clot
Disclosures:
Neil Gambhir indicated no relevant financial relationships.
Samantha Rubin indicated no relevant financial relationships.
Noah Mahpour indicated no relevant financial relationships.
Arun Swaminath: abbvie – Grant/Research Support. janssen – Grant/Research Support.
Neil Gambhir, DO1, Samantha Rubin, DO1, Noah Y. Mahpour, MD1, Arun Swaminath, MD2. P0593 - Underlying Eosinophilic Esophagitis Masquerading as an Upper GI Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
