Sunday Poster Session
Category: Esophagus
P0518 - Evaluating the Effectiveness and Safety of Empiric Esophageal Dilation in Nonobstructive Dysphagia: A Retrospective Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rohit Goyal, MD
Ochsner LSU Health
Shreveport, LA
Presenting Author(s)
Maryam Mubashir, MBBS1, Daniyal Raza, MBBS2, Rohit Goyal, MBBS2, Lena Kawji, MD1, David Okuampa, MD3, Khadija Khan, MD1, Farhan Mohiuddin, MD4, Fatih Gelir, 2, Mohammad Alfrad Nobel Bhuiyan, PhD1, Qiang Cai, MD1, Hassaan A. Zia, MD1
1LSU Health, Shreveport, LA; 2Louisiana State University Health, Shreveport, LA; 3Ochsner LSU Health, Shreveport, LA; 4LSU Health, New Orleans, LA
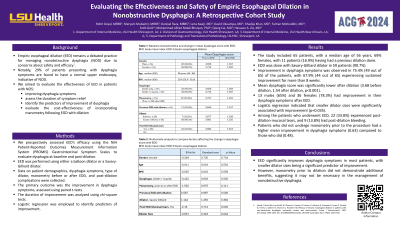
Introduction: Empiric esophageal dilation (EED) remains a debated practice for managing nonobstructive dysphagia (NOD) due to concerns about safety and efficacy. Notably, 29% of patients presenting with dysphagia symptoms are found to have a normal upper endoscopy, indicative of NOD. This study evaluates the effectiveness of EED in improving dysphagia symptoms, assesses the duration of symptom relief, identifies predictors of improvement, and evaluates the cost-effectiveness of incorporating manometry following EGD with dilation.
Methods: We prospectively assessed EED’s efficacy using the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) Gastrointestinal Symptom Scales to evaluate dysphagia at baseline and post-dilation. EED was performed using either a balloon dilator or a Savary-Gilliard dilator. Data on patient demographics, dysphagia symptoms, type of dilator, manometry before or after EDD, and post-dilation complications were collected. The primary outcome was the improvement in dysphagia symptoms, assessed using paired t-tests. The duration of improvement was analyzed using chi-square tests. Logistic regression was employed to identify predictors of improvement.
Results: The study included 65 patients, with a median age of 56 years, 69% females. 11 patients (16.9%) had a previous dilation done, and 59 patients (90.7%) underwent EDD with Savary-Gilliard dilator). Improvement in dysphagia symptoms was observed in 75.4% (49 out of 65) of the patients, with 67.9% (44 out of 65) experiencing sustained improvement for more than 8 weeks. Mean dysphagia score was significantly lower after dilation (3.68 before dilation, 1.54 after dilation, p< 0.001). 13 males (65%) and 36 females (78.3%) had improvement in their dysphagia symptoms after EED. Logistic regression indicated that amongst the dilator sizes the smallest (18mm) were significantly associated with improvement (p=0.035) as this was the most used dilator size. Among the patients who had improvement with EED, 22 (33.8%) experienced post-dilation mucosal tears, and 9 (13.8%) had minor post-dilation bleeding.
Discussion: EED significantly improves dysphagia symptoms in most patients, with smaller dilator sizes being a significant predictor of improvement. However, manometry prior to dilation did not demonstrate additional benefits, suggesting it may not be necessary in the management of nonobstructive dysphagia.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Maryam Mubashir, MBBS1, Daniyal Raza, MBBS2, Rohit Goyal, MBBS2, Lena Kawji, MD1, David Okuampa, MD3, Khadija Khan, MD1, Farhan Mohiuddin, MD4, Fatih Gelir, 2, Mohammad Alfrad Nobel Bhuiyan, PhD1, Qiang Cai, MD1, Hassaan A. Zia, MD1. P0518 - Evaluating the Effectiveness and Safety of Empiric Esophageal Dilation in Nonobstructive Dysphagia: A Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1LSU Health, Shreveport, LA; 2Louisiana State University Health, Shreveport, LA; 3Ochsner LSU Health, Shreveport, LA; 4LSU Health, New Orleans, LA
Introduction: Empiric esophageal dilation (EED) remains a debated practice for managing nonobstructive dysphagia (NOD) due to concerns about safety and efficacy. Notably, 29% of patients presenting with dysphagia symptoms are found to have a normal upper endoscopy, indicative of NOD. This study evaluates the effectiveness of EED in improving dysphagia symptoms, assesses the duration of symptom relief, identifies predictors of improvement, and evaluates the cost-effectiveness of incorporating manometry following EGD with dilation.
Methods: We prospectively assessed EED’s efficacy using the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) Gastrointestinal Symptom Scales to evaluate dysphagia at baseline and post-dilation. EED was performed using either a balloon dilator or a Savary-Gilliard dilator. Data on patient demographics, dysphagia symptoms, type of dilator, manometry before or after EDD, and post-dilation complications were collected. The primary outcome was the improvement in dysphagia symptoms, assessed using paired t-tests. The duration of improvement was analyzed using chi-square tests. Logistic regression was employed to identify predictors of improvement.
Results: The study included 65 patients, with a median age of 56 years, 69% females. 11 patients (16.9%) had a previous dilation done, and 59 patients (90.7%) underwent EDD with Savary-Gilliard dilator). Improvement in dysphagia symptoms was observed in 75.4% (49 out of 65) of the patients, with 67.9% (44 out of 65) experiencing sustained improvement for more than 8 weeks. Mean dysphagia score was significantly lower after dilation (3.68 before dilation, 1.54 after dilation, p< 0.001). 13 males (65%) and 36 females (78.3%) had improvement in their dysphagia symptoms after EED. Logistic regression indicated that amongst the dilator sizes the smallest (18mm) were significantly associated with improvement (p=0.035) as this was the most used dilator size. Among the patients who had improvement with EED, 22 (33.8%) experienced post-dilation mucosal tears, and 9 (13.8%) had minor post-dilation bleeding.
Discussion: EED significantly improves dysphagia symptoms in most patients, with smaller dilator sizes being a significant predictor of improvement. However, manometry prior to dilation did not demonstrate additional benefits, suggesting it may not be necessary in the management of nonobstructive dysphagia.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Maryam Mubashir indicated no relevant financial relationships.
Daniyal Raza indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Lena Kawji indicated no relevant financial relationships.
David Okuampa indicated no relevant financial relationships.
Khadija Khan indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Fatih Gelir indicated no relevant financial relationships.
Mohammad Alfrad Nobel Bhuiyan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Hassaan A. Zia indicated no relevant financial relationships.
Maryam Mubashir, MBBS1, Daniyal Raza, MBBS2, Rohit Goyal, MBBS2, Lena Kawji, MD1, David Okuampa, MD3, Khadija Khan, MD1, Farhan Mohiuddin, MD4, Fatih Gelir, 2, Mohammad Alfrad Nobel Bhuiyan, PhD1, Qiang Cai, MD1, Hassaan A. Zia, MD1. P0518 - Evaluating the Effectiveness and Safety of Empiric Esophageal Dilation in Nonobstructive Dysphagia: A Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
