Sunday Poster Session
Category: Esophagus
P0523 - Combined Anterograde and Retrograde Endoscopic Management of Complete Esophageal Obstruction in Absence of Fluoroscopic Guidance
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Hassaan Arif Maan, MD
Rutgers New Jersey Medical School
Bloomfield, NJ
Presenting Author(s)
Muhammad Hassaan Arif Maan, MD1, Imran A. Qureshi, MD2, Wajiha Khan, MD3, Catherine Choi, MD2, Muhammad Mursaleen Ahmad, MBBS4, Kaveh Hajifathalian, MD2, Weizheng Wang, MD2
1Rutgers New Jersey Medical School, Bloomfield, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Rutgers New Jersey Medical School, Cartaret, NJ; 4Punjab Institute of Medical Sciences, Bloomfield, NJ
Introduction: Head and neck cancers are a relatively common malignancy with radiotherapy as an important component of its management. Esophageal strictures or complete obstruction are major adverse effects of radiotherapy, but can also be caused by acid reflux disease, caustic injury, or Plummer-Vinson syndrome. We describe a case of complete esophageal obstruction, that was successfully managed with combined anterograde and retrograde endoscopic procedure in the absence of fluoroscopic guidance.
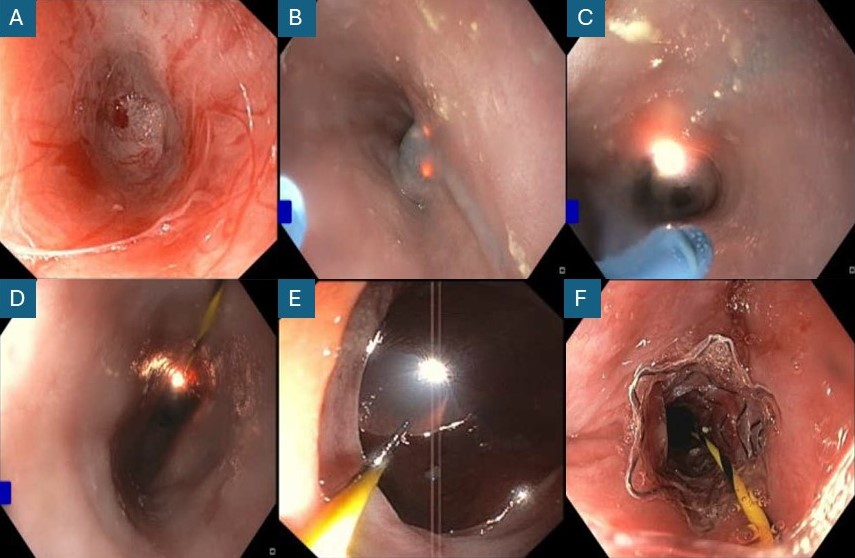
Case Description/Methods: We present a case of a 65-year-old gentleman who had received chemo/radiotherapy for tonsillar cancer and had a gastric tube in place for seven years. He wanted to resume oral intake. Endoscopic evaluation from the gastrostomy site with ultrathin scope demonstrated complete esophageal obstruction at the upper esophageal sphincter. [A] At this point, a rendezvous procedure was planned. One endoscopist used an ultrathin scope to intubate the esophagus from the mouth till the obstruction was noted. Another endoscopist dilated the gastrostomy with a dilator balloon and advanced the gastroscope from the gastrostomy site past the lower esophageal sphincter into the esophagus. The ultrathin scope’s light was visualized through the obstructing mucosa by the gastroscope distal to the obstruction. [B] With direct visualization of transillumination across the obstructing mucosa, a needle knife from the gastroscope was used to cut the obstructing tissue. [C] Following this, a biliary stent was passed over a guidewire and placed over the obstruction site. [D, E, F] A gastrostomy tube was also re-placed. The procedure was performed under general anesthesia and was completed without any complications. The patient was discharged home on a clear liquid diet trial. On postoperative follow-up, the patient denied any procedure complications such as fevers or chest pain secondary to iatrogenic esophageal injury. The patient also endorsed ability to progressively tolerate the liquid diet, with some nausea and acidity with tube feeds.
Discussion: Combined anterograde and retrograde endoscopic intervention is a safe procedure for the management of complete esophageal obstructions. Rendezvous endoscopic procedure can be considered in the absence of fluoroscopy if the obstructing mucosa can be transilluminated and directly visualized by both scopes.
Disclosures:
Muhammad Hassaan Arif Maan, MD1, Imran A. Qureshi, MD2, Wajiha Khan, MD3, Catherine Choi, MD2, Muhammad Mursaleen Ahmad, MBBS4, Kaveh Hajifathalian, MD2, Weizheng Wang, MD2. P0523 - Combined Anterograde and Retrograde Endoscopic Management of Complete Esophageal Obstruction in Absence of Fluoroscopic Guidance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Bloomfield, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Rutgers New Jersey Medical School, Cartaret, NJ; 4Punjab Institute of Medical Sciences, Bloomfield, NJ
Introduction: Head and neck cancers are a relatively common malignancy with radiotherapy as an important component of its management. Esophageal strictures or complete obstruction are major adverse effects of radiotherapy, but can also be caused by acid reflux disease, caustic injury, or Plummer-Vinson syndrome. We describe a case of complete esophageal obstruction, that was successfully managed with combined anterograde and retrograde endoscopic procedure in the absence of fluoroscopic guidance.
Case Description/Methods: We present a case of a 65-year-old gentleman who had received chemo/radiotherapy for tonsillar cancer and had a gastric tube in place for seven years. He wanted to resume oral intake. Endoscopic evaluation from the gastrostomy site with ultrathin scope demonstrated complete esophageal obstruction at the upper esophageal sphincter. [A] At this point, a rendezvous procedure was planned. One endoscopist used an ultrathin scope to intubate the esophagus from the mouth till the obstruction was noted. Another endoscopist dilated the gastrostomy with a dilator balloon and advanced the gastroscope from the gastrostomy site past the lower esophageal sphincter into the esophagus. The ultrathin scope’s light was visualized through the obstructing mucosa by the gastroscope distal to the obstruction. [B] With direct visualization of transillumination across the obstructing mucosa, a needle knife from the gastroscope was used to cut the obstructing tissue. [C] Following this, a biliary stent was passed over a guidewire and placed over the obstruction site. [D, E, F] A gastrostomy tube was also re-placed. The procedure was performed under general anesthesia and was completed without any complications. The patient was discharged home on a clear liquid diet trial. On postoperative follow-up, the patient denied any procedure complications such as fevers or chest pain secondary to iatrogenic esophageal injury. The patient also endorsed ability to progressively tolerate the liquid diet, with some nausea and acidity with tube feeds.
Discussion: Combined anterograde and retrograde endoscopic intervention is a safe procedure for the management of complete esophageal obstructions. Rendezvous endoscopic procedure can be considered in the absence of fluoroscopy if the obstructing mucosa can be transilluminated and directly visualized by both scopes.
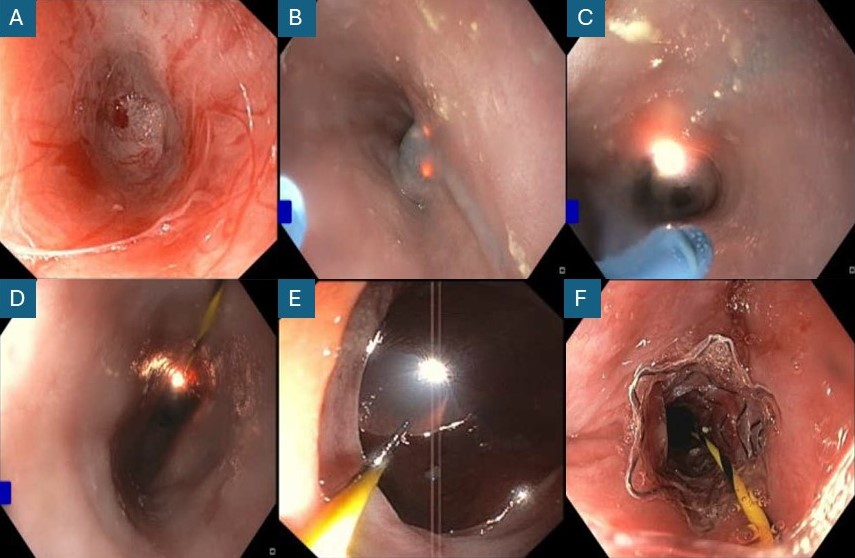
Figure: Figure: Combined anterograde/retrograde resection of esophageal obstructing mucosa
A. Esophageal obstruction being visualized from the proximal ultrathin scope. B. Transillumination across the obstructing mucosa visualized from distal gastroscope. C. Proximal scope visualized by distal scope after resection of obstructing mucosa. D. Distal gastroscope view: Patent esophagus with guidewire after resection of obstructing mucosa. E. Proximal ultrathin scope view: Patent esophagus with guidewire after resection of obstructing mucosa. F. Bare metal stent deployed in the esophagus
A. Esophageal obstruction being visualized from the proximal ultrathin scope. B. Transillumination across the obstructing mucosa visualized from distal gastroscope. C. Proximal scope visualized by distal scope after resection of obstructing mucosa. D. Distal gastroscope view: Patent esophagus with guidewire after resection of obstructing mucosa. E. Proximal ultrathin scope view: Patent esophagus with guidewire after resection of obstructing mucosa. F. Bare metal stent deployed in the esophagus
Disclosures:
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Imran Qureshi indicated no relevant financial relationships.
Wajiha Khan indicated no relevant financial relationships.
Catherine Choi indicated no relevant financial relationships.
Muhammad Mursaleen Ahmad indicated no relevant financial relationships.
Kaveh Hajifathalian indicated no relevant financial relationships.
Weizheng Wang indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan, MD1, Imran A. Qureshi, MD2, Wajiha Khan, MD3, Catherine Choi, MD2, Muhammad Mursaleen Ahmad, MBBS4, Kaveh Hajifathalian, MD2, Weizheng Wang, MD2. P0523 - Combined Anterograde and Retrograde Endoscopic Management of Complete Esophageal Obstruction in Absence of Fluoroscopic Guidance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
