Sunday Poster Session
Category: Esophagus
P0531 - An Uncommon Case of Metastatic Breast Cancer to the Esophagus Causing Pseudoachalasia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Teskey Garrett, DO
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Teskey Garrett, DO1, Alex Prevallet, DO2, Rohit Khanna, DO3, Franklin Tsai, MD4, Walter Coyle, MD4
1Scripps Mercy Hospital, San Diego, CA; 2HCA Riverside Community Hospital, Riverside, CA; 3Scripps Green Hospital, San Diego, CA; 4Scripps Green Hospital, La Jolla, CA
Introduction: Pseudoachalasia manifests from both benign and malignant processes at the gastroesophageal junction (GEJ). This is a 65-year-old woman with recurrent breast cancer who presented with dysphagia and esophageal wall thickening initially suggesting achalasia. However, endosonography (EUS) guided biopsy demonstrated pseudoachalasia due to metastatic breast cancer.
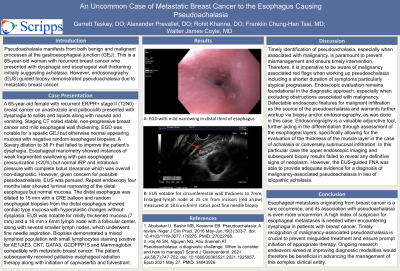
Case Description/Methods: A A 65-year-old female with recurrent ER/PR+ stage II (T2N0) breast cancer on anastrozole and palbociclib presented with dysphagia to solids and liquids along with nausea and vomiting. Staging CT noted stable, non-progressive breast cancer and mild esophageal wall thickening. EGD was notable for a spastic GEJ but otherwise normal appearing mucosa with negative random esophageal biopsies. A Savary dilation to 36 Fr that failed to improve the patient’s dysphagia. Esophageal manometry showed instances of weak fragmented swallowing with pan-esophageal pressurization (< 20%) but normal IRP and intrabolus pressure with complete bolus clearance which was overall non-diagnostic. However, given concern for possible pseudoachalasia, EUS was pursued. Repeat endoscopy four months later showed luminal narrowing of the distal esophagus but normal mucosa. The distal esophagus was dilated to 15 mm with a CRE balloon and random esophageal biopsies from the distal esophagus showed cardiac type mucosa with hyperplastic changes without dysplasia. EUS was notable for mildly thickened mucosa (7 mm) and a 18 mm x 6mm lymph node with a follicular center, along with several smaller lymph nodes, which underwent fine needle aspiration. Biopsies demonstrated a mixed lymphoid population with small lymphocytes staining positive for AE1/AE3, CK7, GATA3, GCDFPP15 and Mammaglobin compatible with metastatic breast cancer. The patient subsequently received palliative esophageal radiation therapy along with initiation of capivasertib and fulvestrant.
Discussion: Esophageal metastasis originating from breast cancer is a rare occurrence, and its association with pseudoachalasia is even more uncommon. A high index of suspicion for esophageal metastases is needed when encountering dysphagia in patients with breast cancer. Timely recognition of malignancy-associated pseudoachalasia is crucial to prevent misguided treatment and ensure prompt initiation of appropriate therapy. Ongoing research endeavors aimed at improving diagnostic modalities would therefore be beneficial in advancing the management of this complex clinical entity.

Disclosures:
Teskey Garrett, DO1, Alex Prevallet, DO2, Rohit Khanna, DO3, Franklin Tsai, MD4, Walter Coyle, MD4. P0531 - An Uncommon Case of Metastatic Breast Cancer to the Esophagus Causing Pseudoachalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Scripps Mercy Hospital, San Diego, CA; 2HCA Riverside Community Hospital, Riverside, CA; 3Scripps Green Hospital, San Diego, CA; 4Scripps Green Hospital, La Jolla, CA
Introduction: Pseudoachalasia manifests from both benign and malignant processes at the gastroesophageal junction (GEJ). This is a 65-year-old woman with recurrent breast cancer who presented with dysphagia and esophageal wall thickening initially suggesting achalasia. However, endosonography (EUS) guided biopsy demonstrated pseudoachalasia due to metastatic breast cancer.
Case Description/Methods: A A 65-year-old female with recurrent ER/PR+ stage II (T2N0) breast cancer on anastrozole and palbociclib presented with dysphagia to solids and liquids along with nausea and vomiting. Staging CT noted stable, non-progressive breast cancer and mild esophageal wall thickening. EGD was notable for a spastic GEJ but otherwise normal appearing mucosa with negative random esophageal biopsies. A Savary dilation to 36 Fr that failed to improve the patient’s dysphagia. Esophageal manometry showed instances of weak fragmented swallowing with pan-esophageal pressurization (< 20%) but normal IRP and intrabolus pressure with complete bolus clearance which was overall non-diagnostic. However, given concern for possible pseudoachalasia, EUS was pursued. Repeat endoscopy four months later showed luminal narrowing of the distal esophagus but normal mucosa. The distal esophagus was dilated to 15 mm with a CRE balloon and random esophageal biopsies from the distal esophagus showed cardiac type mucosa with hyperplastic changes without dysplasia. EUS was notable for mildly thickened mucosa (7 mm) and a 18 mm x 6mm lymph node with a follicular center, along with several smaller lymph nodes, which underwent fine needle aspiration. Biopsies demonstrated a mixed lymphoid population with small lymphocytes staining positive for AE1/AE3, CK7, GATA3, GCDFPP15 and Mammaglobin compatible with metastatic breast cancer. The patient subsequently received palliative esophageal radiation therapy along with initiation of capivasertib and fulvestrant.
Discussion: Esophageal metastasis originating from breast cancer is a rare occurrence, and its association with pseudoachalasia is even more uncommon. A high index of suspicion for esophageal metastases is needed when encountering dysphagia in patients with breast cancer. Timely recognition of malignancy-associated pseudoachalasia is crucial to prevent misguided treatment and ensure prompt initiation of appropriate therapy. Ongoing research endeavors aimed at improving diagnostic modalities would therefore be beneficial in advancing the management of this complex clinical entity.

Figure: EUS notable for circumferential esophageal wall thickening to 7mm. Enlarged lymph node at 25 cm from incisors (red arrow) measured at 18.6 x 6.6mm status post fine needle biopsy
Disclosures:
Teskey Garrett indicated no relevant financial relationships.
Alex Prevallet indicated no relevant financial relationships.
Rohit Khanna indicated no relevant financial relationships.
Franklin Tsai indicated no relevant financial relationships.
Walter Coyle indicated no relevant financial relationships.
Teskey Garrett, DO1, Alex Prevallet, DO2, Rohit Khanna, DO3, Franklin Tsai, MD4, Walter Coyle, MD4. P0531 - An Uncommon Case of Metastatic Breast Cancer to the Esophagus Causing Pseudoachalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
