Sunday Poster Session
Category: Esophagus
P0532 - The Worst of Both Worlds: Adenosquamous Carcinoma of the Esophagus
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rachael Hagen, DO
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rachael Hagen, DO1, Minh Thu T.. Nguyen, MD2, Danzhu Zhao, DO2, Rishabh Sachdev, MD2
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT
Introduction: Esophageal cancer is the 6th leading cause of cancer-related deaths. Its primary forms are adenocarcinoma (AC) and squamous cell carcinoma (SCC). Esophageal adenosquamous carcinoma (EASC), a rare subtype composed of both AC and SCC elements, represents less than 1% of esophageal cancers. EASC is aggressive, with a 5-year survival rate of 45.2% for localized disease and 4.8% for cases with distant metastasis. Here, we report a rare case of adenosquamous carcinoma in a long-term smoker.
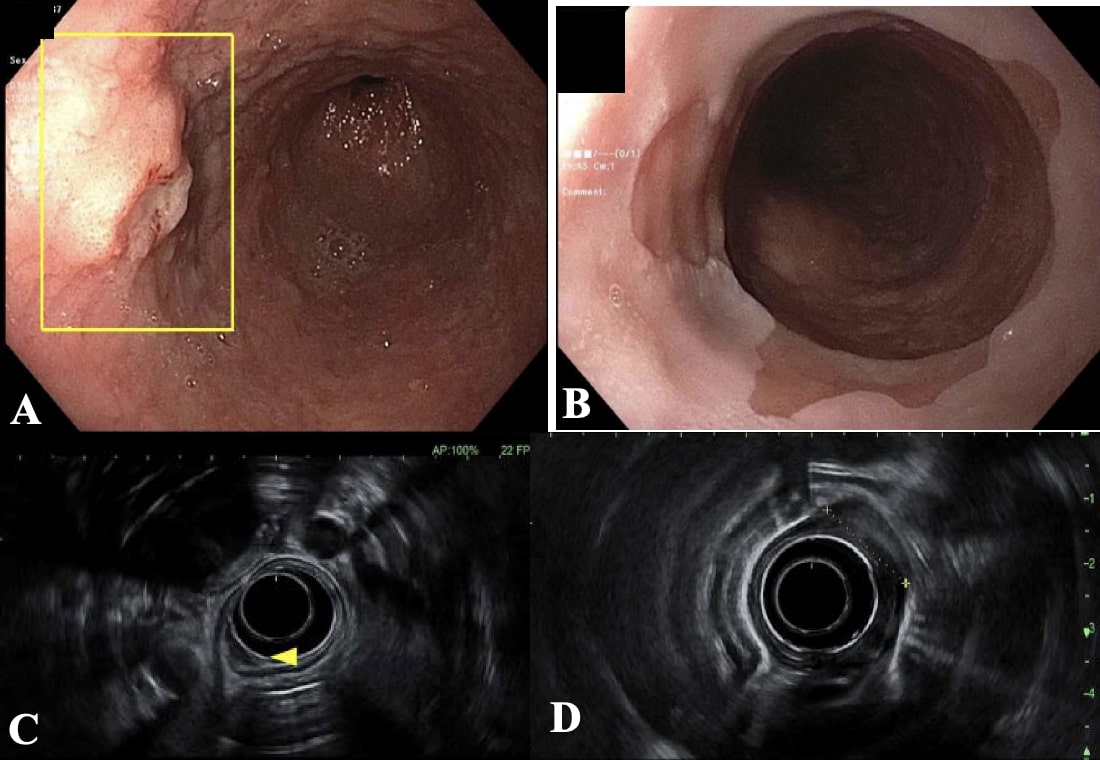
Case Description/Methods: A 59-year-old female presented with a two-year history of progressive dysphagia to solids and liquids, accompanied by a 40-pound weight loss. She reported consuming 6 beers weekly and had a 46 pack-year smoking history. Esophagogastroduodenoscopy (EGD) revealed a 15-cm segment of Barrett's esophagus, along with an ulcerated mass in the mid-esophagus (Fig. 1a-b). Pathology confirmed invasive EASC with 80% SCC and 20% AC components.
Endoscopic ultrasound (EUS) indicated a T2N1 lesion involving the muscularis propria layer (Fig. 1c-d). Computed tomography (CT) of the thorax and abdomen detected a 5-mm right paraoesophageal lymph node. Positron emission tomography (PET)-CT showed mild fluorodeoxyglucose activity within the esophagus without distant metastatic disease. She received a diagnosis of EASC (cT2N1M0) and began neoadjuvant chemoradiation with carboplatin/paclitaxel, with plans for surgical resection based on a favorable response on repeat PET-CT.
Discussion: The origin of EASC remains unclear, although it is often associated with Barrett’s esophagus, though rates are ill-defined. This association is likely due to the genetic loss of heterozygosity, missense mutations, and reflux-induced metaplasia. In this case, dysplastic Barrett’s esophagus increased her likelihood of developing AC, while her smoking and alcohol use further elevated her risk for SCC.
EASC is often misdiagnosed as SCC due to sampling errors, as the AC component typically lies deeper than the mucosal SCC component. An invasive growth pattern is often observed endoscopically. For disease staging, EUS is considered the gold standard. CT should be performed to assess for metastatic involvement, followed by PET/CT. Recognizing this rare entity is important, given the poor prognosis, necessitating prompt intervention with chemotherapy, radiation, and/or surgery. Further research is needed to better understand the pathogenesis and to establish optimal treatment strategies.
Disclosures:
Rachael Hagen, DO1, Minh Thu T.. Nguyen, MD2, Danzhu Zhao, DO2, Rishabh Sachdev, MD2. P0532 - The Worst of Both Worlds: Adenosquamous Carcinoma of the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT
Introduction: Esophageal cancer is the 6th leading cause of cancer-related deaths. Its primary forms are adenocarcinoma (AC) and squamous cell carcinoma (SCC). Esophageal adenosquamous carcinoma (EASC), a rare subtype composed of both AC and SCC elements, represents less than 1% of esophageal cancers. EASC is aggressive, with a 5-year survival rate of 45.2% for localized disease and 4.8% for cases with distant metastasis. Here, we report a rare case of adenosquamous carcinoma in a long-term smoker.
Case Description/Methods: A 59-year-old female presented with a two-year history of progressive dysphagia to solids and liquids, accompanied by a 40-pound weight loss. She reported consuming 6 beers weekly and had a 46 pack-year smoking history. Esophagogastroduodenoscopy (EGD) revealed a 15-cm segment of Barrett's esophagus, along with an ulcerated mass in the mid-esophagus (Fig. 1a-b). Pathology confirmed invasive EASC with 80% SCC and 20% AC components.
Endoscopic ultrasound (EUS) indicated a T2N1 lesion involving the muscularis propria layer (Fig. 1c-d). Computed tomography (CT) of the thorax and abdomen detected a 5-mm right paraoesophageal lymph node. Positron emission tomography (PET)-CT showed mild fluorodeoxyglucose activity within the esophagus without distant metastatic disease. She received a diagnosis of EASC (cT2N1M0) and began neoadjuvant chemoradiation with carboplatin/paclitaxel, with plans for surgical resection based on a favorable response on repeat PET-CT.
Discussion: The origin of EASC remains unclear, although it is often associated with Barrett’s esophagus, though rates are ill-defined. This association is likely due to the genetic loss of heterozygosity, missense mutations, and reflux-induced metaplasia. In this case, dysplastic Barrett’s esophagus increased her likelihood of developing AC, while her smoking and alcohol use further elevated her risk for SCC.
EASC is often misdiagnosed as SCC due to sampling errors, as the AC component typically lies deeper than the mucosal SCC component. An invasive growth pattern is often observed endoscopically. For disease staging, EUS is considered the gold standard. CT should be performed to assess for metastatic involvement, followed by PET/CT. Recognizing this rare entity is important, given the poor prognosis, necessitating prompt intervention with chemotherapy, radiation, and/or surgery. Further research is needed to better understand the pathogenesis and to establish optimal treatment strategies.
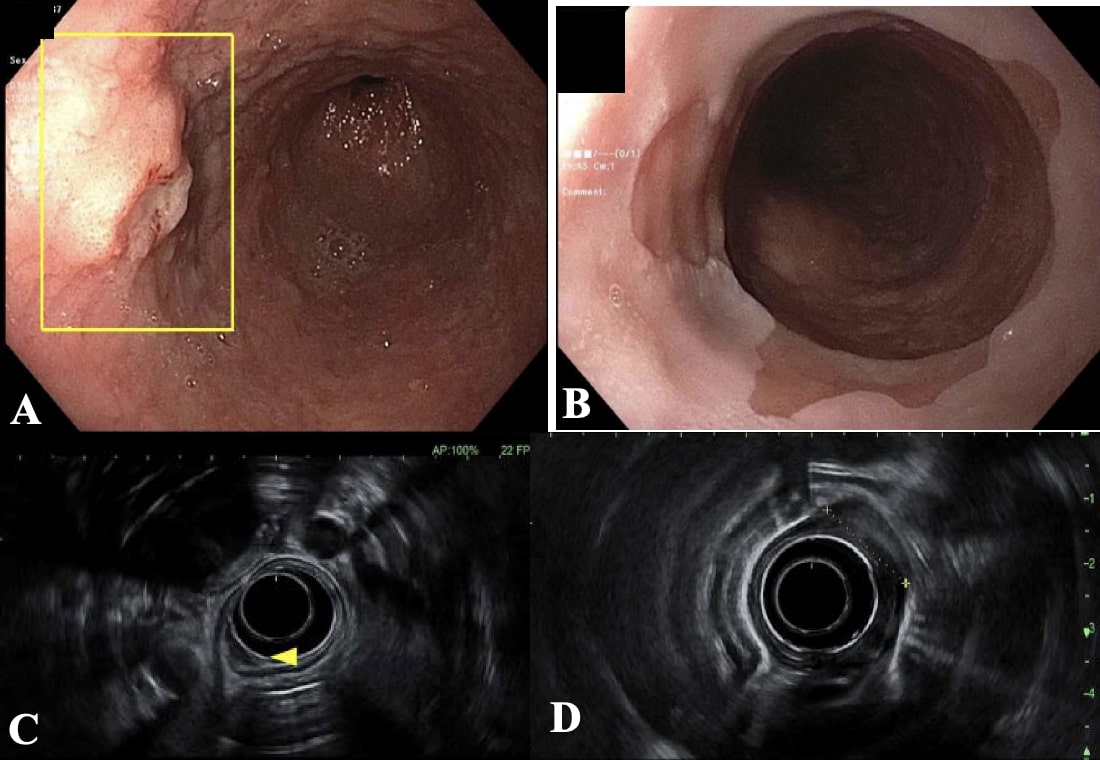
Figure: Figure 1.
EGD showed an ulcerated mass in the lower third of the esophagus (a). Esophageal mucosal changes consistent with long-segment Barrett’s esophagus were seen extending from the upper gastric folds to the Z-line, measuring up to 15 cm (b).
EUS visualized an intramural lesion in the cervical and upper third of the esophagus with poorly defined borders and invasion into the submucosa (c). A hypoechoic mass was seen in the thoracic esophagus and middle third of the esophagus with invasion into the deep mucosa with wall thickening involving the muscularis propria layer (d).
EGD showed an ulcerated mass in the lower third of the esophagus (a). Esophageal mucosal changes consistent with long-segment Barrett’s esophagus were seen extending from the upper gastric folds to the Z-line, measuring up to 15 cm (b).
EUS visualized an intramural lesion in the cervical and upper third of the esophagus with poorly defined borders and invasion into the submucosa (c). A hypoechoic mass was seen in the thoracic esophagus and middle third of the esophagus with invasion into the deep mucosa with wall thickening involving the muscularis propria layer (d).
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Danzhu Zhao indicated no relevant financial relationships.
Rishabh Sachdev indicated no relevant financial relationships.
Rachael Hagen, DO1, Minh Thu T.. Nguyen, MD2, Danzhu Zhao, DO2, Rishabh Sachdev, MD2. P0532 - The Worst of Both Worlds: Adenosquamous Carcinoma of the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
