Sunday Poster Session
Category: Endoscopy Video Forum
P0458 - Leveraging Regenerative Biotherapeutics: A Novel Approach to Chronic Fistula Closure
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JT
Jaclyn Tuck, MD
Mayo Clinic
Phoenix, AZ
Presenting Author(s)
Jaclyn Tuck, MD1, Danial Shaikh, MD1, Lisa Rotellini-Coltvet, PA-C1, Norio Fukami, MD1, Grace Knuttinen, MD, PhD1, Rahul Pannala, MD2
1Mayo Clinic, Phoenix, AZ; 2Mayo Clinic, Scottsdale, AZ
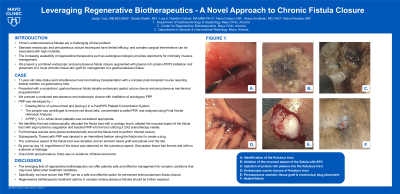
Introduction: Chronic enterocutaneous fistulae are a challenging clinical problem. Standard endoscopic and percutaneous closure techniques have limited efficacy and complex surgical interventions can be associated with high morbidity. The increasing availability of regenerative therapeutics such as autologous biologics provides opportunity for minimally invasive management. We present a combined endoscopic and percutaneous fistula closure augmented with platelet rich plasma (PRP) instillation and placement of a novel amniotic tissue skin graft for management of a recalcitrant gastrocutaneous fistula.
Case Description/Methods: A 71-year-old man status-post simultaneous heart and kidney transplantation with a complex post-transplant course requiring enteral nutrition via gastrostomy tube, presented with a recalcitrant gastrocutaneous fistula despite endoscopic gastric suture closure and percutaneous mechanical plug placement. Therefore, we pursued a combined percutaneous and endoscopic closure with instillation of autologous PRP. PRP was developed by drawing 60mL of venous blood and placing it in a PurePrPII Platelet Concentration System. The sample was centrifuged to remove red blood cells, concentrated to pellet PRP, and analyzed using Final Horiba Hemolytic Analyzer. A PRP 3-5 x whole blood platelets was considered appropriate. We identified the tract endoscopically, denuded the fistula tract with a cytology brush, ablated the mucosal aspect of the fistula tract with argon plasma coagulation and injected PRP into the tract utilizing a 23G sclerotherapy needle. Full thickness sutures were placed endoscopically around the fistula tract to perform internal closure. Subsequently, Tisseel with PRP was injected in an intermittent fashion along the fistula tract to create a plug. The cutaneous aspect of the fistula tract was abraded, and an amniotic tissue graft was placed over the site. By post-op day 16, engraftment of the tissue was observed on the cutaneous aspect. Granulation tissue had formed and with no evidence of drainage. One-month post-procedure, there was no evidence of fistula recurrence.
Discussion: The emerging field of regenerative biotherapeutics can offer patients safe and effective management for complex conditions that may have failed other treatment modalities. Specifically, we have shown that PRP can be a safe and effective option for permanent enterocutaneous fistula closure. Regenerative biotherapeutic treatment options in complex enterocutaneous fistulae should be further explored.
Disclosures:
Jaclyn Tuck, MD1, Danial Shaikh, MD1, Lisa Rotellini-Coltvet, PA-C1, Norio Fukami, MD1, Grace Knuttinen, MD, PhD1, Rahul Pannala, MD2. P0458 - Leveraging Regenerative Biotherapeutics: A Novel Approach to Chronic Fistula Closure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Phoenix, AZ; 2Mayo Clinic, Scottsdale, AZ
Introduction: Chronic enterocutaneous fistulae are a challenging clinical problem. Standard endoscopic and percutaneous closure techniques have limited efficacy and complex surgical interventions can be associated with high morbidity. The increasing availability of regenerative therapeutics such as autologous biologics provides opportunity for minimally invasive management. We present a combined endoscopic and percutaneous fistula closure augmented with platelet rich plasma (PRP) instillation and placement of a novel amniotic tissue skin graft for management of a recalcitrant gastrocutaneous fistula.
Case Description/Methods: A 71-year-old man status-post simultaneous heart and kidney transplantation with a complex post-transplant course requiring enteral nutrition via gastrostomy tube, presented with a recalcitrant gastrocutaneous fistula despite endoscopic gastric suture closure and percutaneous mechanical plug placement. Therefore, we pursued a combined percutaneous and endoscopic closure with instillation of autologous PRP. PRP was developed by drawing 60mL of venous blood and placing it in a PurePrPII Platelet Concentration System. The sample was centrifuged to remove red blood cells, concentrated to pellet PRP, and analyzed using Final Horiba Hemolytic Analyzer. A PRP 3-5 x whole blood platelets was considered appropriate. We identified the tract endoscopically, denuded the fistula tract with a cytology brush, ablated the mucosal aspect of the fistula tract with argon plasma coagulation and injected PRP into the tract utilizing a 23G sclerotherapy needle. Full thickness sutures were placed endoscopically around the fistula tract to perform internal closure. Subsequently, Tisseel with PRP was injected in an intermittent fashion along the fistula tract to create a plug. The cutaneous aspect of the fistula tract was abraded, and an amniotic tissue graft was placed over the site. By post-op day 16, engraftment of the tissue was observed on the cutaneous aspect. Granulation tissue had formed and with no evidence of drainage. One-month post-procedure, there was no evidence of fistula recurrence.
Discussion: The emerging field of regenerative biotherapeutics can offer patients safe and effective management for complex conditions that may have failed other treatment modalities. Specifically, we have shown that PRP can be a safe and effective option for permanent enterocutaneous fistula closure. Regenerative biotherapeutic treatment options in complex enterocutaneous fistulae should be further explored.
Disclosures:
Jaclyn Tuck indicated no relevant financial relationships.
Danial Shaikh indicated no relevant financial relationships.
Lisa Rotellini-Coltvet indicated no relevant financial relationships.
Norio Fukami indicated no relevant financial relationships.
Grace Knuttinen indicated no relevant financial relationships.
Rahul Pannala: HCL Technologies – Consultant. Nestle Healthsciences – Advisor or Review Panel Member.
Jaclyn Tuck, MD1, Danial Shaikh, MD1, Lisa Rotellini-Coltvet, PA-C1, Norio Fukami, MD1, Grace Knuttinen, MD, PhD1, Rahul Pannala, MD2. P0458 - Leveraging Regenerative Biotherapeutics: A Novel Approach to Chronic Fistula Closure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
