Sunday Poster Session
Category: Colon
P0357 - Outpatient Management of Small Bowel Perforation: A Case Report and Review of Literature
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sagar Nagpal, MD
East Tennessee State University Quillen College of Medicine
Johnson City, TN
Presenting Author(s)
Sagar Nagpal, MD, David Berry, DO, Hezborn Magacha, MD, MPH, Diana Nunley-Gorman, MD
East Tennessee State University Quillen College of Medicine, Johnson City, TN
Introduction: Small bowel perforation denotes a disruption in the integrity of the small bowel wall, which may stem from various factors such as trauma, iatrogenic causes, diverticular perforation, duodenal ulcer, ischemia, or neoplasms. The management guidelines for diverticular perforation in the small bowel remain unclear. Treatment options typically encompass surgical intervention or a conservative approach. Herein, we report the case of a 75-year-old woman presenting with duodenal diverticular perforation, which was managed conservatively in the outpatient setting.
Case Description/Methods: A 75-year-old woman, with a past medical history of diverticulosis and chronic constipation, presented to the primary care clinic with worsening abdominal pain. She described two days of progressive epigastric pain radiating to her left abdomen and shoulder, accompanied by fever, nausea, and bloating. Despite using over-the-counter antacids, she found no relief.
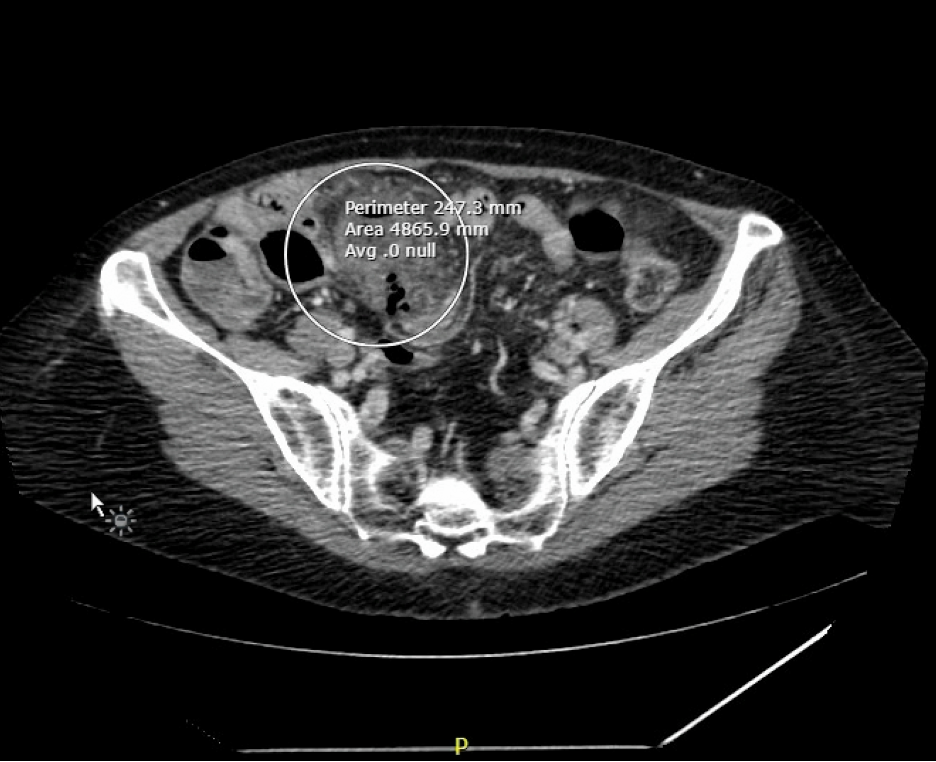
Physical examination revealed diffuse abdominal tenderness, particularly in the left lower quadrant, with normal findings elsewhere. Laboratory tests indicated an elevated white cell count of 13.13 (normal range of 3.4-10.8 10*3uL). A Computed tomography scan (CT scan) of the abdomen confirmed small bowel diverticulitis with an adjacent focus of gas in the mesentery consistent with micro-perforation (Image 1). Scattered diverticulosis of the descending and sigmoid colon was noted, but the large bowel was otherwise unremarkable.
We decided for outpatient management due to her stable condition. She was prescribed a 7-day course of oral antibiotics with ciprofloxacin and metronidazole, along with instructions to maintain oral hydration, follow a low-residue diet, and suspend her constipation medication.
The patient's condition improved over time. Follow-up CT after 3 weeks showed improving inflammatory changes surrounding the previous micro perforation site. Extraluminal pockets of air representing micro perforation had resolved. On further follow-up, the patient showed clinical improvement.
Discussion: Duodenal diverticular perforation presents a rare yet life-threatening complication with diverse clinical manifestations. Conservative management of small bowel perforation in an outpatient setting may be appropriate for hemodynamically stable patients without signs of sepsis, peritonitis, or significant comorbidities. Close monitoring is essential to track symptom improvement and ensure patient well-being.
Disclosures:
Sagar Nagpal, MD, David Berry, DO, Hezborn Magacha, MD, MPH, Diana Nunley-Gorman, MD. P0357 - Outpatient Management of Small Bowel Perforation: A Case Report and Review of Literature, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
East Tennessee State University Quillen College of Medicine, Johnson City, TN
Introduction: Small bowel perforation denotes a disruption in the integrity of the small bowel wall, which may stem from various factors such as trauma, iatrogenic causes, diverticular perforation, duodenal ulcer, ischemia, or neoplasms. The management guidelines for diverticular perforation in the small bowel remain unclear. Treatment options typically encompass surgical intervention or a conservative approach. Herein, we report the case of a 75-year-old woman presenting with duodenal diverticular perforation, which was managed conservatively in the outpatient setting.
Case Description/Methods: A 75-year-old woman, with a past medical history of diverticulosis and chronic constipation, presented to the primary care clinic with worsening abdominal pain. She described two days of progressive epigastric pain radiating to her left abdomen and shoulder, accompanied by fever, nausea, and bloating. Despite using over-the-counter antacids, she found no relief.
Physical examination revealed diffuse abdominal tenderness, particularly in the left lower quadrant, with normal findings elsewhere. Laboratory tests indicated an elevated white cell count of 13.13 (normal range of 3.4-10.8 10*3uL). A Computed tomography scan (CT scan) of the abdomen confirmed small bowel diverticulitis with an adjacent focus of gas in the mesentery consistent with micro-perforation (Image 1). Scattered diverticulosis of the descending and sigmoid colon was noted, but the large bowel was otherwise unremarkable.
We decided for outpatient management due to her stable condition. She was prescribed a 7-day course of oral antibiotics with ciprofloxacin and metronidazole, along with instructions to maintain oral hydration, follow a low-residue diet, and suspend her constipation medication.
The patient's condition improved over time. Follow-up CT after 3 weeks showed improving inflammatory changes surrounding the previous micro perforation site. Extraluminal pockets of air representing micro perforation had resolved. On further follow-up, the patient showed clinical improvement.
Discussion: Duodenal diverticular perforation presents a rare yet life-threatening complication with diverse clinical manifestations. Conservative management of small bowel perforation in an outpatient setting may be appropriate for hemodynamically stable patients without signs of sepsis, peritonitis, or significant comorbidities. Close monitoring is essential to track symptom improvement and ensure patient well-being.
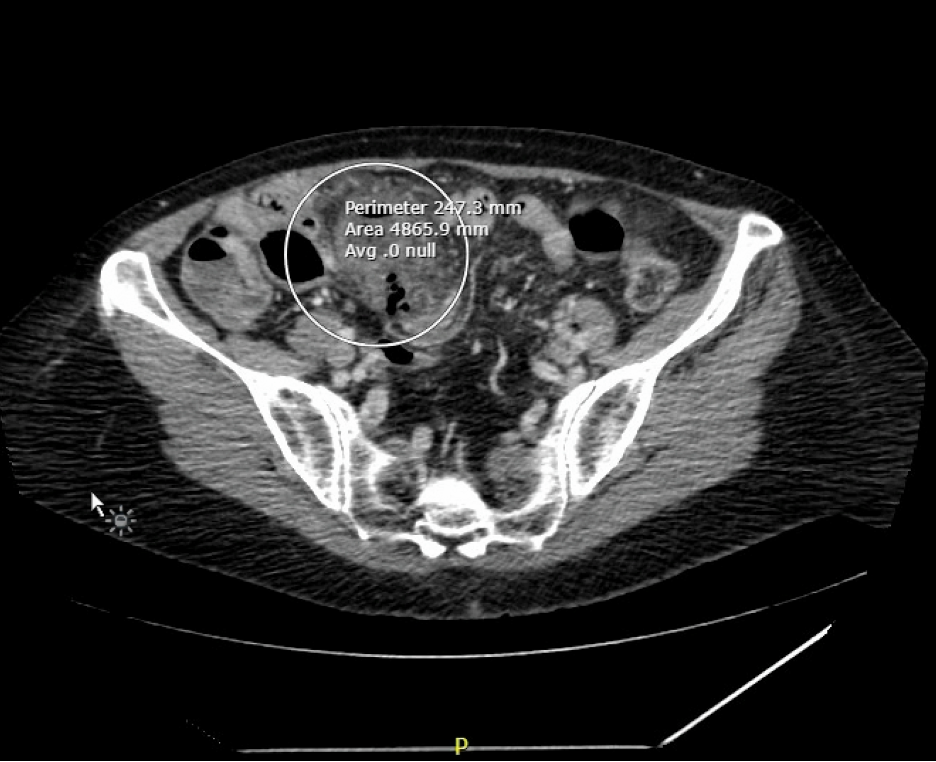
Figure: Computed tomography (CT) scan of the abdomen showing small bowel diverticulitis with an air leak from small bowel perforation.
Disclosures:
Sagar Nagpal indicated no relevant financial relationships.
David Berry indicated no relevant financial relationships.
Hezborn Magacha indicated no relevant financial relationships.
Diana Nunley-Gorman indicated no relevant financial relationships.
Sagar Nagpal, MD, David Berry, DO, Hezborn Magacha, MD, MPH, Diana Nunley-Gorman, MD. P0357 - Outpatient Management of Small Bowel Perforation: A Case Report and Review of Literature, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
