Sunday Poster Session
Category: Colon
P0365 - A Case of Severe Amebiasis in a Patient With Sarcoidosis on Low-dose Immunosuppressive Steroid Therapy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Mohamed K. Osman, MD, MPH
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Award: Presidential Poster Award
Mohamed K.. Osman, MD, MPH, Thin Phyu Phyu Aung, MD, Marina Landa, MD, Alvaro Genao, MD, Joan Culpepper-Morgan, MD, FACG
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Amebic colitis is rare in the USA. Immigrants and travelers to endemic countries are at risk of infection. High-dose corticosteroids are known to be immunosuppressive and precipitate severe amebiasis. We report a case of low-dose steroid therapy causing severe amebic colitis.
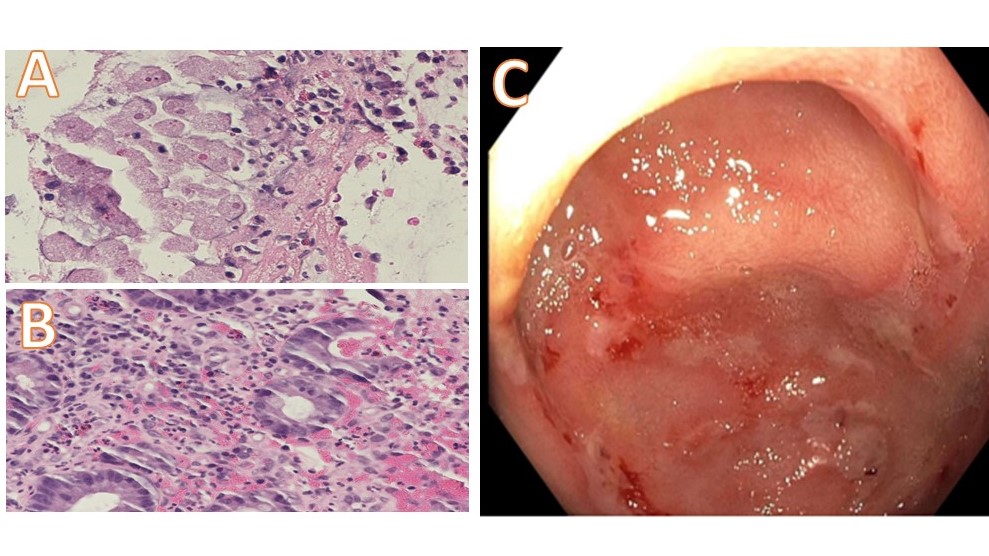
Case Description/Methods: A 43-year-old Senegalese man, who immigrated to the USA 11 months ago, was diagnosed with stage-4 lung sarcoidosis 4 months before presentation. Upon diagnosis prednisone 10 mg daily was started and had tapered to 2.5 mg daily when he presented with bloody diarrhea and epigastric pain for 3 months. Exam revealed a thin body habitus. WBC count was 5.04 K/uL, hemoglobin 14.1 g/dl, and platelets 350 K/uL. Neutrophil percentage was 55.7%, lymphocytes 19.4%, monocytes 17.5% (NR 2-14%), and eosinophils 6.2% (NR 1-4%). HIV and QuantiFERON tests were negative. Colonoscopy showed a scattered area of moderately erythematous, friable, scarred, congested, and ulcerated mucosa with yellow exudates throughout and patchy mildly erythema in the sigmoid. Right colon biopsy showed fragments of benign colonic mucosa and granulation tissue, suggestive of ulcer with Entameba histolytica (EH) present and necrotic tissue. Left colon biopsy showed focal mild, and rectum moderate non-specific chronic active colitis with no granuloma or dysplasia (Figure 1). Terminal ileum biopsy was normal. P-ANCA was negative, ASCA IgG 97 units, and IgA 16.8 units (NR< 20). A diagnosis of severe amebic colitis was made and managed with metronidazole. By 2 months follow-up, his symptoms had resolved. Ova/parasites and GI-PCR panels were negative. EH antibodies were positive. CRP was 5 mg/L (NR 0-4 mg/L) and ESR 12 (NR 0-15 mm/hr). A course of paromomycin was given.
Discussion: Amebic infections are mostly asymptomatic with 10% progressing to watery diarrhea, bloody diarrhea, and abdominal pain. Fulminant colitis with leukocytosis, toxic megacolon, necrosis, perforation, and peritonitis has a 40% mortality. Immunosuppression due to steroids or chemotherapy is reported as a risk for fulminant amebic colitis. The doses given this patient and the slow pace of steroid taper make the emergence of infection unusual. The positive ASCA IgG posits Crohn’s Disease. However, the histology and onset with the start of steroid therapy makes this unlikely. Our case highlights that, like tuberculosis, latent amebiasis may be reactivated in those with a history of travel to endemic regions, even with low-dose steroid therapy.
Disclosures:
Mohamed K.. Osman, MD, MPH, Thin Phyu Phyu Aung, MD, Marina Landa, MD, Alvaro Genao, MD, Joan Culpepper-Morgan, MD, FACG. P0365 - A Case of Severe Amebiasis in a Patient With Sarcoidosis on Low-dose Immunosuppressive Steroid Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mohamed K.. Osman, MD, MPH, Thin Phyu Phyu Aung, MD, Marina Landa, MD, Alvaro Genao, MD, Joan Culpepper-Morgan, MD, FACG
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Amebic colitis is rare in the USA. Immigrants and travelers to endemic countries are at risk of infection. High-dose corticosteroids are known to be immunosuppressive and precipitate severe amebiasis. We report a case of low-dose steroid therapy causing severe amebic colitis.
Case Description/Methods: A 43-year-old Senegalese man, who immigrated to the USA 11 months ago, was diagnosed with stage-4 lung sarcoidosis 4 months before presentation. Upon diagnosis prednisone 10 mg daily was started and had tapered to 2.5 mg daily when he presented with bloody diarrhea and epigastric pain for 3 months. Exam revealed a thin body habitus. WBC count was 5.04 K/uL, hemoglobin 14.1 g/dl, and platelets 350 K/uL. Neutrophil percentage was 55.7%, lymphocytes 19.4%, monocytes 17.5% (NR 2-14%), and eosinophils 6.2% (NR 1-4%). HIV and QuantiFERON tests were negative. Colonoscopy showed a scattered area of moderately erythematous, friable, scarred, congested, and ulcerated mucosa with yellow exudates throughout and patchy mildly erythema in the sigmoid. Right colon biopsy showed fragments of benign colonic mucosa and granulation tissue, suggestive of ulcer with Entameba histolytica (EH) present and necrotic tissue. Left colon biopsy showed focal mild, and rectum moderate non-specific chronic active colitis with no granuloma or dysplasia (Figure 1). Terminal ileum biopsy was normal. P-ANCA was negative, ASCA IgG 97 units, and IgA 16.8 units (NR< 20). A diagnosis of severe amebic colitis was made and managed with metronidazole. By 2 months follow-up, his symptoms had resolved. Ova/parasites and GI-PCR panels were negative. EH antibodies were positive. CRP was 5 mg/L (NR 0-4 mg/L) and ESR 12 (NR 0-15 mm/hr). A course of paromomycin was given.
Discussion: Amebic infections are mostly asymptomatic with 10% progressing to watery diarrhea, bloody diarrhea, and abdominal pain. Fulminant colitis with leukocytosis, toxic megacolon, necrosis, perforation, and peritonitis has a 40% mortality. Immunosuppression due to steroids or chemotherapy is reported as a risk for fulminant amebic colitis. The doses given this patient and the slow pace of steroid taper make the emergence of infection unusual. The positive ASCA IgG posits Crohn’s Disease. However, the histology and onset with the start of steroid therapy makes this unlikely. Our case highlights that, like tuberculosis, latent amebiasis may be reactivated in those with a history of travel to endemic regions, even with low-dose steroid therapy.
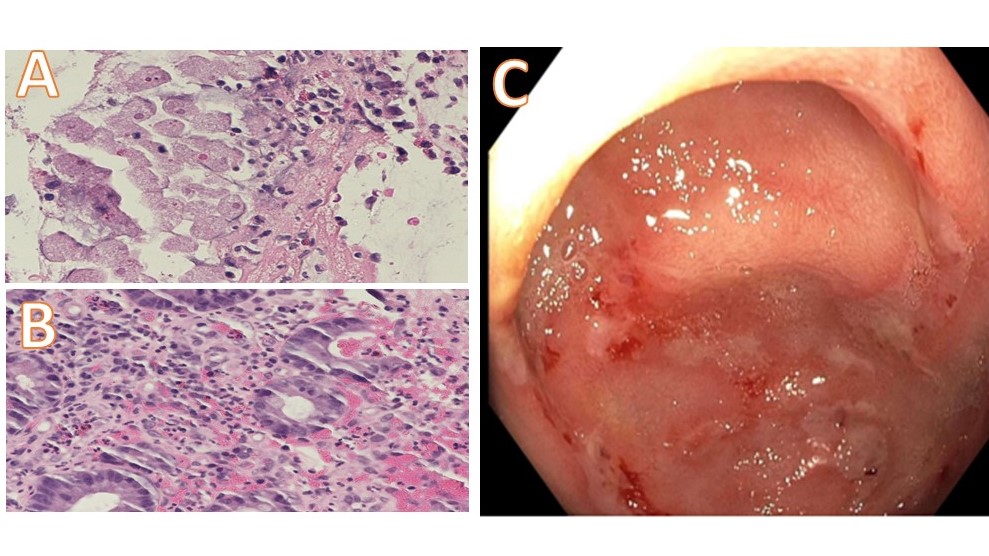
Figure: A: Entameba histolytica organisms with foamy cytoplasm containing eccentric nuclei and red blood cells, granulation tissue suggesting ulcer, and necrosis on right colon biopsy. B: Moderate non-specific chronic active colitis with no granuloma, or dysplasia. C: Friable, erythematous, congested and ulcerated mucosa with yellow exudates.
Disclosures:
Mohamed Osman indicated no relevant financial relationships.
Thin Phyu Phyu Aung indicated no relevant financial relationships.
Marina Landa indicated no relevant financial relationships.
Alvaro Genao indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Mohamed K.. Osman, MD, MPH, Thin Phyu Phyu Aung, MD, Marina Landa, MD, Alvaro Genao, MD, Joan Culpepper-Morgan, MD, FACG. P0365 - A Case of Severe Amebiasis in a Patient With Sarcoidosis on Low-dose Immunosuppressive Steroid Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

