Sunday Poster Session
Category: Colon
P0257 - Severe Cytomegalovirus Proctitis in an Immunocompetent Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rachael Hagen, DO
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rachael Hagen, DO1, Teresa Da Cunha, MD2, Alexander Potashinsky, MD3
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3Hartford Healthcare, New Britain, CT
Introduction: Cytomegalovirus (CMV) may cause infections in immunocompromised patients but rarely causes disease in immunocompetent hosts. Moreover, few cases of CMV proctitis have been reported, which manifests as colitis with rectal pain and bleeding. Here, we report a case of an immunocompetent man who presented with hematochezia and was found to have severe CMV proctitis despite no known risk factors.
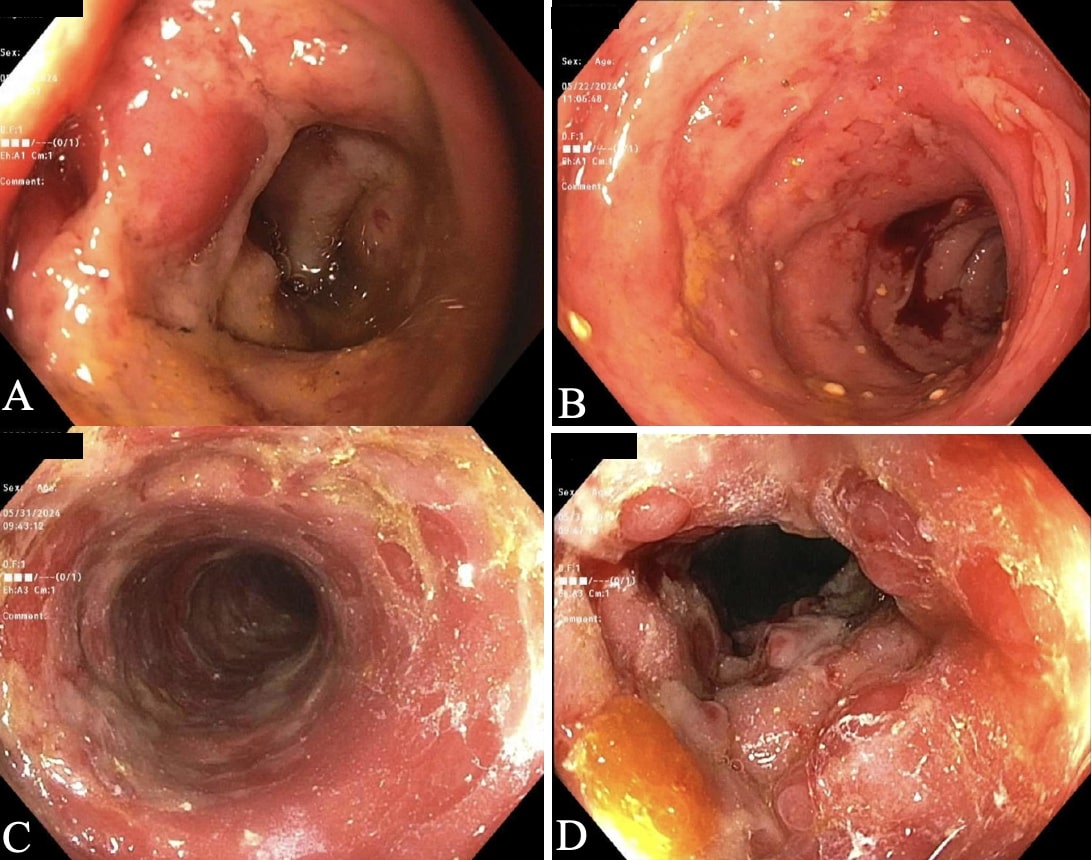
Case Description/Methods: A 71-year-old male presented with 2 days of left lower quadrant abdominal pain, hematochezia, and fevers. He was diagnosed with Rotavirus and Norovirus colitis and was discharged. He re-presented 3 days later as symptoms continued. Computed tomography (CT) abdomen/pelvis redemonstrated sigmoid and rectal thickening. Erythrocyte sedimentation rate was normal, C-reactive protein was elevated to 1.94 mg/dL and fecal calprotectin was elevated to >8000 mc/g. Clostridium difficile testing was negative. Endoscopy showed erythematous and friable mucosa with bleeding in the rectum and sigmoid colon (Fig. 1a). Biopsies showed acute inflammation, staining for CMV was negative.
He did not improve despite treatment with antibiotics, budesonide, and mesalamine. He denied a history of anal intercourse. Human immunodeficiency virus (HIV), herpes simplex virus, chlamydia, and gonorrhea serologies were negative. Repeat imaging one week later showed worsening colitis of the sigmoid colon and rectum. Endoscopy revealed severe congestion with hemorrhagic and ulcerated mucosa in the rectum, sigmoid, and descending colon (Fig. 1b). Biopsies showed ulcerated and acutely inflamed rectosigmoid colitis, positive for CMV. He was treated with ganciclovir with symptomatic improvement and advised to undergo repeat endoscopy to monitor response.
Discussion: CMV proctitis is rare in immunocompetent individuals but should be considered when patients present with rectal pain, hematochezia, and mononucleosis-like symptoms. Risk factors include immunosuppression, anal intercourse, and primary CMV infection, but the cause in this case remains unclear. Ulcerations and mucositis may be visualized endoscopically. CMV serology and biopsy are confirmatory. Common causes of colitis should be ruled out, such as C. difficile, inflammatory bowel disease, ischemic colitis, and sexually transmitted diseases. Screening for HIV is also indicated given the strong association with HIV. CMV proctitis often resolves spontaneously, but severe cases require treatment with ganciclovir or valganciclovir due to the high mortality rate.
Disclosures:
Rachael Hagen, DO1, Teresa Da Cunha, MD2, Alexander Potashinsky, MD3. P0257 - Severe Cytomegalovirus Proctitis in an Immunocompetent Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3Hartford Healthcare, New Britain, CT
Introduction: Cytomegalovirus (CMV) may cause infections in immunocompromised patients but rarely causes disease in immunocompetent hosts. Moreover, few cases of CMV proctitis have been reported, which manifests as colitis with rectal pain and bleeding. Here, we report a case of an immunocompetent man who presented with hematochezia and was found to have severe CMV proctitis despite no known risk factors.
Case Description/Methods: A 71-year-old male presented with 2 days of left lower quadrant abdominal pain, hematochezia, and fevers. He was diagnosed with Rotavirus and Norovirus colitis and was discharged. He re-presented 3 days later as symptoms continued. Computed tomography (CT) abdomen/pelvis redemonstrated sigmoid and rectal thickening. Erythrocyte sedimentation rate was normal, C-reactive protein was elevated to 1.94 mg/dL and fecal calprotectin was elevated to >8000 mc/g. Clostridium difficile testing was negative. Endoscopy showed erythematous and friable mucosa with bleeding in the rectum and sigmoid colon (Fig. 1a). Biopsies showed acute inflammation, staining for CMV was negative.
He did not improve despite treatment with antibiotics, budesonide, and mesalamine. He denied a history of anal intercourse. Human immunodeficiency virus (HIV), herpes simplex virus, chlamydia, and gonorrhea serologies were negative. Repeat imaging one week later showed worsening colitis of the sigmoid colon and rectum. Endoscopy revealed severe congestion with hemorrhagic and ulcerated mucosa in the rectum, sigmoid, and descending colon (Fig. 1b). Biopsies showed ulcerated and acutely inflamed rectosigmoid colitis, positive for CMV. He was treated with ganciclovir with symptomatic improvement and advised to undergo repeat endoscopy to monitor response.
Discussion: CMV proctitis is rare in immunocompetent individuals but should be considered when patients present with rectal pain, hematochezia, and mononucleosis-like symptoms. Risk factors include immunosuppression, anal intercourse, and primary CMV infection, but the cause in this case remains unclear. Ulcerations and mucositis may be visualized endoscopically. CMV serology and biopsy are confirmatory. Common causes of colitis should be ruled out, such as C. difficile, inflammatory bowel disease, ischemic colitis, and sexually transmitted diseases. Screening for HIV is also indicated given the strong association with HIV. CMV proctitis often resolves spontaneously, but severe cases require treatment with ganciclovir or valganciclovir due to the high mortality rate.
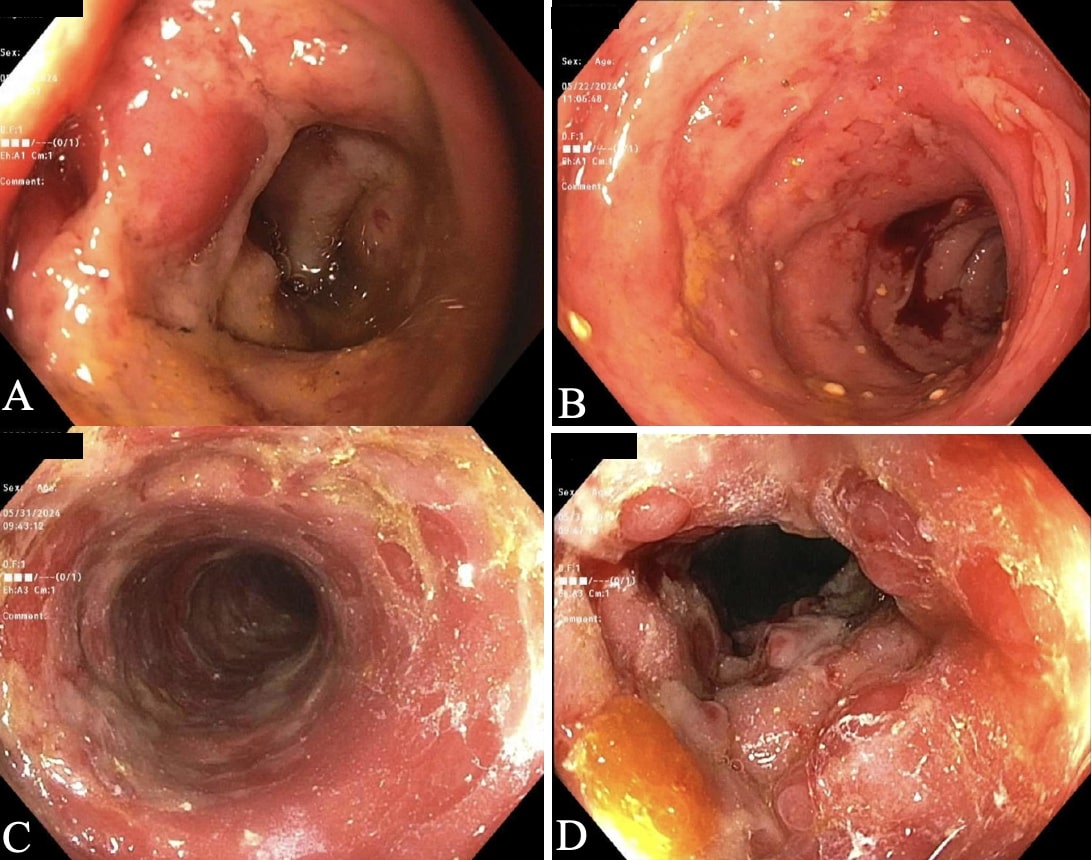
Figure: Figure 1a. Flexible sigmoidoscopy demonstrated erythematous and friable mucosa with contact bleeding in the rectum and sigmoid colon.
Figure 1b. Flexible sigmoidoscopy a week later revealed more severe congestion with hemorrhagic, inflamed, and ulcerated mucosa in the rectum, sigmoid, and descending colon.
Figure 1b. Flexible sigmoidoscopy a week later revealed more severe congestion with hemorrhagic, inflamed, and ulcerated mucosa in the rectum, sigmoid, and descending colon.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Teresa Da Cunha indicated no relevant financial relationships.
Alexander Potashinsky indicated no relevant financial relationships.
Rachael Hagen, DO1, Teresa Da Cunha, MD2, Alexander Potashinsky, MD3. P0257 - Severe Cytomegalovirus Proctitis in an Immunocompetent Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
