Sunday Poster Session
Category: Colon
P0271 - Acute Ischemic Colitis Secondary to Inferior Mesenteric Arteriovenous Malformation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MB
Madeline Vithya Barnaba Durairaj, MBBS, MD, DM
UNC Health Blue Ridge
Prairie Village, KS
Presenting Author(s)
Madeline Vithya Barnaba Durairaj, MBBS, MD, DM1, Hamid Reza Moein, MD2, Lisa McKinney, DO2, Patricia Amoako, MD2
1UNC Health Blue Ridge, Prairie Village, KS; 2UNC Health Blue Ridge, Morganton, NC
Introduction: Ischemic colitis is the most common form of gastrointestinal ischemia, occurring secondary to occlusive or non-occlusive etiology. Its presentation as acute large bowel diarrhea secondary to arteriovenous malformation is quite rare. We present a rare case of acute ischemic colitis secondary to inferior mesenteric arteriovenous malformation.
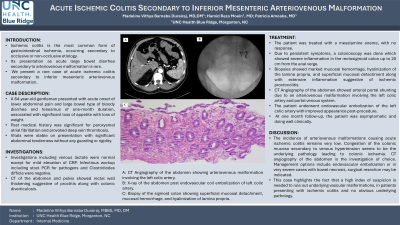
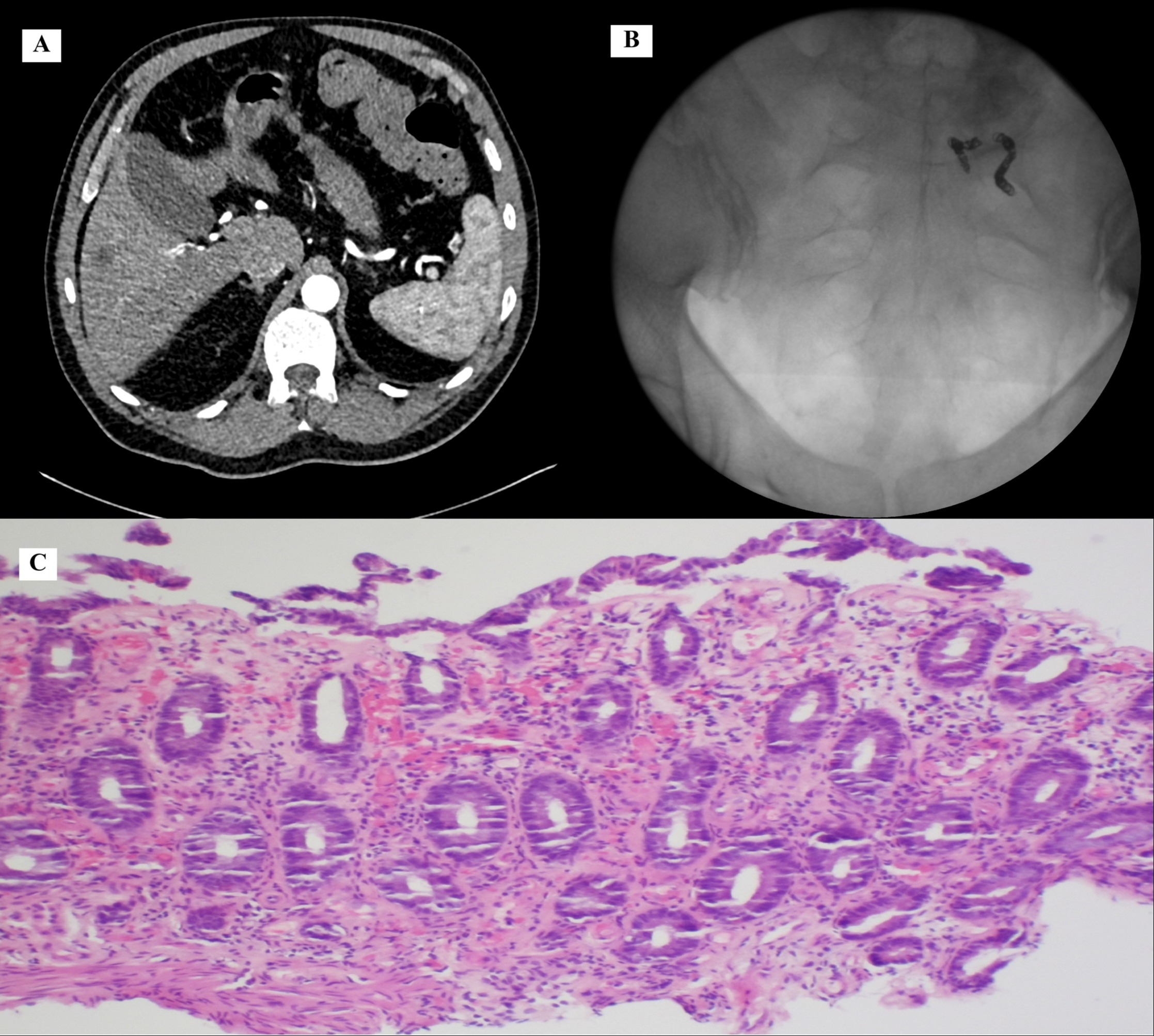
Case Description/Methods: A 64-year-old gentleman presented with acute onset of lower abdominal pain and large bowel type of bloody diarrhea and tenesmus of one-month duration, associated with significant loss of appetite with loss of weight. He reported no similar episodes in the past. Past medical history was significant for paroxysmal atrial fibrillation and provoked deep vein thrombosis. Vitals were stable on presentation with significant abdominal tenderness without any guarding or rigidity. Investigations including venous lactate were normal except for mild elevation of CRP. Infectious workup including stool PCR for pathogens and Clostridiodes difficle were negative. CT of the abdomen and pelvis showed rectal wall thickening suggestive of proctitis along with colonic diverticulosis. The patient was treated with a mesalamine enema, with no response. Due to persistent symptoms, a colonoscopy was done which showed severe inflammation in the rectosigmoid colon up to 20 cm from the anal verge. Biopsies showed marked mucosal hemorrhage, hyalinization of the lamina propria, and superficial mucosal detachment along with extensive inflammation suggestive of ischemic proctocolitis. CT Angiography of the abdomen showed arterial portal shunting due to an arteriovenous malformation involving the left colic artery and portal venous system. The patient underwent endovascular embolization of the left colic artery with improved appearance post-procedure. At one month follow-up, the patient was asymptomatic and doing well clinically.
Discussion: The incidence of arteriovenous malformations causing acute ischemic colitis remains very low. Congestion of the colonic mucosa secondary to venous hypertension seems to be the underlying pathology leading to colonic ischemia. CT angiography of the abdomen is the investigation of choice. Management options include endovascular embolization or in very severe cases with bowel necrosis, surgical resection may be indicated. This case highlights the fact that a high index of suspicion is needed to rule out underlying vascular malformations, in patients presenting with ischemic colitis and no obvious underlying pathology.
Disclosures:
Madeline Vithya Barnaba Durairaj, MBBS, MD, DM1, Hamid Reza Moein, MD2, Lisa McKinney, DO2, Patricia Amoako, MD2. P0271 - Acute Ischemic Colitis Secondary to Inferior Mesenteric Arteriovenous Malformation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UNC Health Blue Ridge, Prairie Village, KS; 2UNC Health Blue Ridge, Morganton, NC
Introduction: Ischemic colitis is the most common form of gastrointestinal ischemia, occurring secondary to occlusive or non-occlusive etiology. Its presentation as acute large bowel diarrhea secondary to arteriovenous malformation is quite rare. We present a rare case of acute ischemic colitis secondary to inferior mesenteric arteriovenous malformation.
Case Description/Methods: A 64-year-old gentleman presented with acute onset of lower abdominal pain and large bowel type of bloody diarrhea and tenesmus of one-month duration, associated with significant loss of appetite with loss of weight. He reported no similar episodes in the past. Past medical history was significant for paroxysmal atrial fibrillation and provoked deep vein thrombosis. Vitals were stable on presentation with significant abdominal tenderness without any guarding or rigidity. Investigations including venous lactate were normal except for mild elevation of CRP. Infectious workup including stool PCR for pathogens and Clostridiodes difficle were negative. CT of the abdomen and pelvis showed rectal wall thickening suggestive of proctitis along with colonic diverticulosis. The patient was treated with a mesalamine enema, with no response. Due to persistent symptoms, a colonoscopy was done which showed severe inflammation in the rectosigmoid colon up to 20 cm from the anal verge. Biopsies showed marked mucosal hemorrhage, hyalinization of the lamina propria, and superficial mucosal detachment along with extensive inflammation suggestive of ischemic proctocolitis. CT Angiography of the abdomen showed arterial portal shunting due to an arteriovenous malformation involving the left colic artery and portal venous system. The patient underwent endovascular embolization of the left colic artery with improved appearance post-procedure. At one month follow-up, the patient was asymptomatic and doing well clinically.
Discussion: The incidence of arteriovenous malformations causing acute ischemic colitis remains very low. Congestion of the colonic mucosa secondary to venous hypertension seems to be the underlying pathology leading to colonic ischemia. CT angiography of the abdomen is the investigation of choice. Management options include endovascular embolization or in very severe cases with bowel necrosis, surgical resection may be indicated. This case highlights the fact that a high index of suspicion is needed to rule out underlying vascular malformations, in patients presenting with ischemic colitis and no obvious underlying pathology.
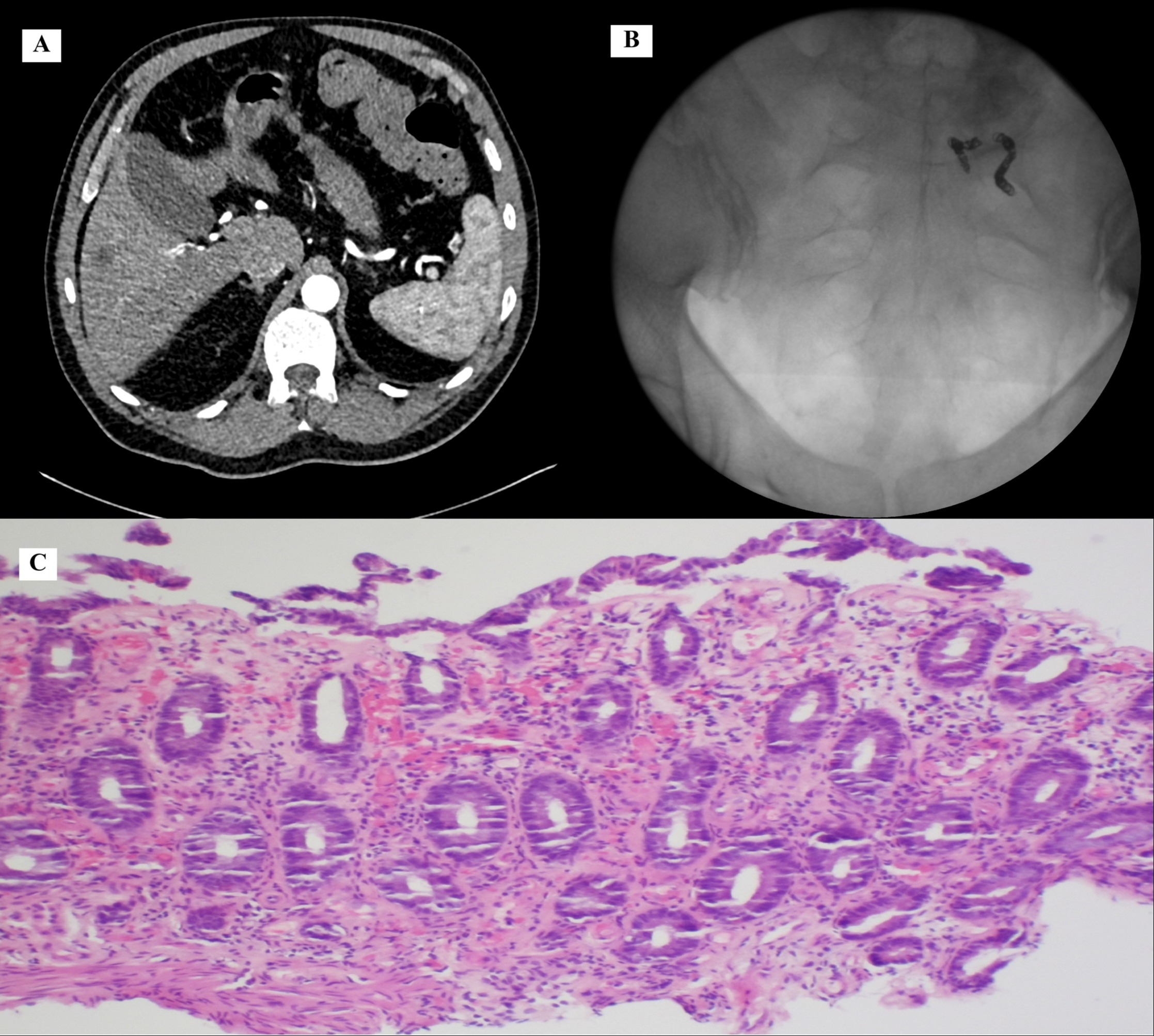
Figure: A - CT Angiography of the abdomen showing arteriovenous malformation involving the left colic artery.
B - X-ray of the abdomen post endovascular coil embolization of left colic artery.
C - Biopsy of the sigmoid colon showing superficial mucosal detachment, mucosal hemorrhage, and hyalinization of lamina propia.
B - X-ray of the abdomen post endovascular coil embolization of left colic artery.
C - Biopsy of the sigmoid colon showing superficial mucosal detachment, mucosal hemorrhage, and hyalinization of lamina propia.
Disclosures:
Madeline Vithya Barnaba Durairaj indicated no relevant financial relationships.
Hamid Reza Moein indicated no relevant financial relationships.
Lisa McKinney indicated no relevant financial relationships.
Patricia Amoako indicated no relevant financial relationships.
Madeline Vithya Barnaba Durairaj, MBBS, MD, DM1, Hamid Reza Moein, MD2, Lisa McKinney, DO2, Patricia Amoako, MD2. P0271 - Acute Ischemic Colitis Secondary to Inferior Mesenteric Arteriovenous Malformation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
