Sunday Poster Session
Category: Colon
P0276 - From Hole to Whole: A Case Report on Recto-Neovaginal Fistula Resolution With Endorectal Advancement Flap in Gender Affirming Surgery Complications
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Oaksoe Aung, BS
University of California Davis School of Medicine
Temple City, CA
Presenting Author(s)
Oaksoe Aung, BS1, Sean Michael Flynn, MD2
1University of California Davis School of Medicine, Temple City, CA; 2University of California Davis Medical Center, Sacramento, CA
Introduction: Recto-neovaginal fistulas (RnVFs) are uncommon yet challenging complications following gender-affirming surgery, characterized by an abnormal communication between the rectum and neovagina. Incidence rates range from 2%-17%. Management strategies vary, including primary closure, diverting colostomies, and endorectal advancement flap (ERAF). Despite promising outcomes, literature on ERAF efficacy in RnVF management remains limited. This case report details the successful treatment of a RnVF in a 20-year-old transgender individual using ERAF, contributing to the understanding and management for this condition.
Case Description/Methods: A 20-year-old transgender woman developed a RnVF following gender-affirming surgery, presenting with pelvic discomfort, constipation, and rectal bleeding. Initial management involved a diverting colostomy to reduce perineal inflammation and sepsis, protecting the neovaginal reconstruction. Exam under anesthesia (EUA) identified a 1.5 cm fistula proximal to the levator complex. Definitive management included ERAF, where a 2 cm x 6 cm partial thickness flap was raised from the rectal side, unhealthy tissue debrided, and the defect closed with running 2-0 PDS sutures. The mucosal flap was advanced and secured with interrupted 2-0 Vicryl sutures. The procedure achieved successful fistula closure without complications. Post-op follow-ups confirmed healing, with a well-functioning colostomy and resolved symptoms. Final EUA with an air leak test confirmed the absence of recurrence, validating the effectiveness of the ERAF procedure.
Discussion: This case report demonstrates the successful use of ERAF in managing a RnVF in a transgender woman post-gender-affirming surgery. The patient's favorable outcome, facilitated by a young age and the absence of Crohn's disease, underscores the potential of ERAF as a viable treatment modality. Consistent with existing literature, our approach highlighted the necessity of complete excision of the fistula tract, effective mucosal advancement, and diligent postoperative care. Our case report reinforces the importance of a multidisciplinary approach involving colorectal surgeons and transgender healthcare specialists. Long-term follow-up and prospective studies with larger sample sizes are essential to further elucidate the factors influencing ERAF success in this patient population. By sharing our experience, we aim to inform clinical practice and contribute to the growing body of knowledge on managing RnVFs in transgender patients.
Disclosures:
Oaksoe Aung, BS1, Sean Michael Flynn, MD2. P0276 - From Hole to Whole: A Case Report on Recto-Neovaginal Fistula Resolution With Endorectal Advancement Flap in Gender Affirming Surgery Complications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California Davis School of Medicine, Temple City, CA; 2University of California Davis Medical Center, Sacramento, CA
Introduction: Recto-neovaginal fistulas (RnVFs) are uncommon yet challenging complications following gender-affirming surgery, characterized by an abnormal communication between the rectum and neovagina. Incidence rates range from 2%-17%. Management strategies vary, including primary closure, diverting colostomies, and endorectal advancement flap (ERAF). Despite promising outcomes, literature on ERAF efficacy in RnVF management remains limited. This case report details the successful treatment of a RnVF in a 20-year-old transgender individual using ERAF, contributing to the understanding and management for this condition.
Case Description/Methods: A 20-year-old transgender woman developed a RnVF following gender-affirming surgery, presenting with pelvic discomfort, constipation, and rectal bleeding. Initial management involved a diverting colostomy to reduce perineal inflammation and sepsis, protecting the neovaginal reconstruction. Exam under anesthesia (EUA) identified a 1.5 cm fistula proximal to the levator complex. Definitive management included ERAF, where a 2 cm x 6 cm partial thickness flap was raised from the rectal side, unhealthy tissue debrided, and the defect closed with running 2-0 PDS sutures. The mucosal flap was advanced and secured with interrupted 2-0 Vicryl sutures. The procedure achieved successful fistula closure without complications. Post-op follow-ups confirmed healing, with a well-functioning colostomy and resolved symptoms. Final EUA with an air leak test confirmed the absence of recurrence, validating the effectiveness of the ERAF procedure.
Discussion: This case report demonstrates the successful use of ERAF in managing a RnVF in a transgender woman post-gender-affirming surgery. The patient's favorable outcome, facilitated by a young age and the absence of Crohn's disease, underscores the potential of ERAF as a viable treatment modality. Consistent with existing literature, our approach highlighted the necessity of complete excision of the fistula tract, effective mucosal advancement, and diligent postoperative care. Our case report reinforces the importance of a multidisciplinary approach involving colorectal surgeons and transgender healthcare specialists. Long-term follow-up and prospective studies with larger sample sizes are essential to further elucidate the factors influencing ERAF success in this patient population. By sharing our experience, we aim to inform clinical practice and contribute to the growing body of knowledge on managing RnVFs in transgender patients.
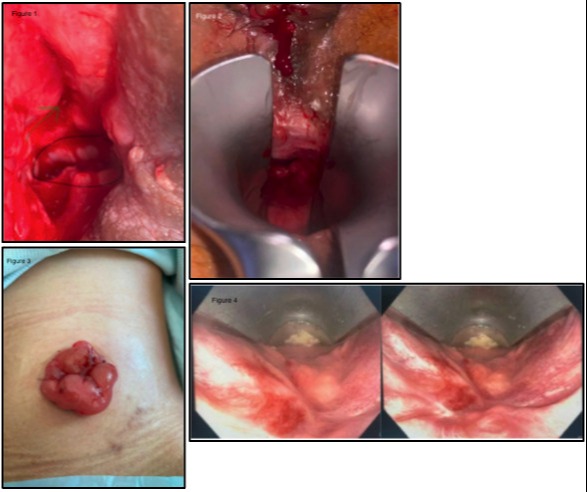
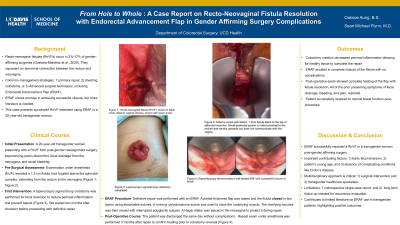
Figure: Figure 1 : Recto-neovaginal fistula (RnVF), shown in black circle, distal to vaginal introitus, shown with green arrow.
Figure 2 : Anterior rectal wall defect, 1.5cm fistula distal to the top of sphincter muscles. Small peri-rectal pocket is noted proximal to the rectum that travels upwards but does not communicate with the vagina.
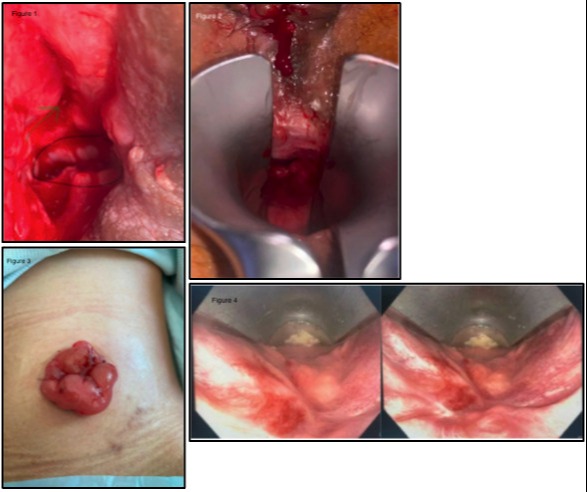
Figure 3 : Laparoscopic sigmoid loop colostomy completed.
Figure 4 : Sigmoidoscopy demonstrates a well healed Endorectal Advancement Flap (ERAF) with successful closure of RnVF.
Figure 2 : Anterior rectal wall defect, 1.5cm fistula distal to the top of sphincter muscles. Small peri-rectal pocket is noted proximal to the rectum that travels upwards but does not communicate with the vagina.
Figure 3 : Laparoscopic sigmoid loop colostomy completed.
Figure 4 : Sigmoidoscopy demonstrates a well healed Endorectal Advancement Flap (ERAF) with successful closure of RnVF.
Disclosures:
Oaksoe Aung indicated no relevant financial relationships.
Sean Michael Flynn indicated no relevant financial relationships.
Oaksoe Aung, BS1, Sean Michael Flynn, MD2. P0276 - From Hole to Whole: A Case Report on Recto-Neovaginal Fistula Resolution With Endorectal Advancement Flap in Gender Affirming Surgery Complications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
