Sunday Poster Session
Category: Biliary/Pancreas
P0183 - Refractory Neuroglycopenia and Hyperinsulinemia: An Unusual Case of Metastatic Pancreatic Neuroendocrine Tumor
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Samier Deen, DO
HonorHealth
Scottsdale, AZ
Presenting Author(s)
Samier Deen, DO1, Ahmed Abidali, DO2, Jacob T. Harris, MD1, Faisal Mehmood, MD1, Gavin Levinthal, MD1, Bassel Al-Lahham, MD3
1HonorHealth, Scottsdale, AZ; 2Abrazo Health, Glendale, AZ; 3HonorHealth, Phoenix, AZ
Introduction: Metastatic insulinoma, a rare form of pancreatic neuroendocrine tumor (panNET), is hypothesized to originate from non-functioning panNETs. Malignant transformation and hepatic metastasis are highly unusual features, accounting for only a fraction of panNET cases. Symptoms are often attributed to refractory hypoglycemia, including confusion, headaches, and diarrhea. Endoscopic ultrasonography (EUS) is a viable diagnostic modality in cases where pancreatic lesions are indiscernible on CT, but suspicion is high. Treatment often includes somatostatin analogues (SSA) and chemotherapy, resulting in resolution of hypoglycemia.
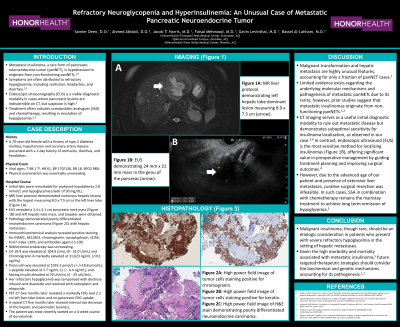
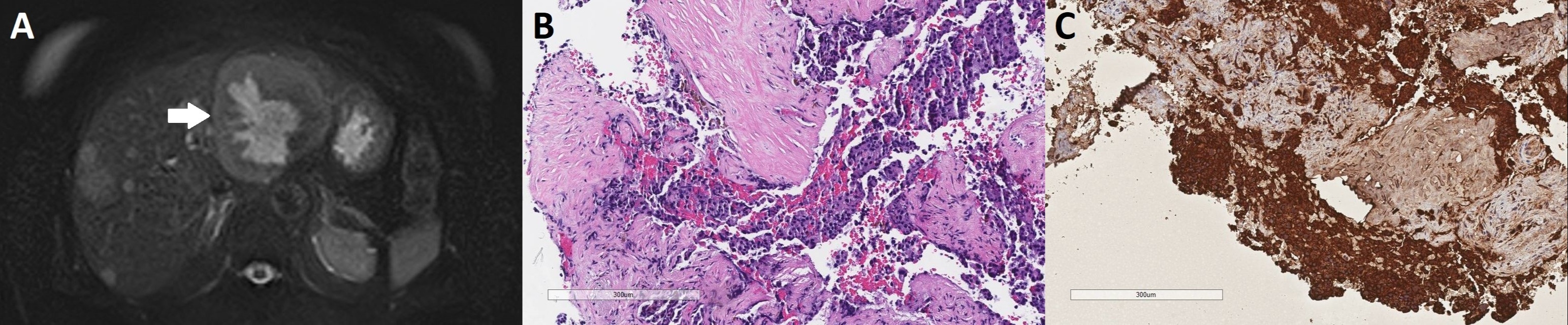
Case Description/Methods: A 70-year-old female with a history of type 2 diabetes mellitus, hypertension and coronary artery disease presented with a 1-day history of confusion, diarrhea, and headaches. Initial labs were remarkable for profound hypokalemia and hypoglycemia (nadir of 30 mg/dL). MRI liver protocol demonstrated numerous hepatic lesions with the largest measuring 8.0 x 7.5 cm in the left liver lobe. EUS revealed a 2.4 x 2.1 cm pancreatic neck mass and left hepatic lobe mass, and biopsies were obtained. Bidirectional endoscopy was unrevealing. Pathology demonstrated poorly differentiated neuroendocrine carcinoma with hepatic metastasis. Immunohistochemical analysis revealed positive staining for INSM1, AE1/AE3, chromogranin, synaptophysin, CD56, Ki-67 index >20%, and antibodies against S-100. CA 19-9, fasting insulin, proinsulin, and c-peptide levels were markedly elevated. Her refractory hypoglycemia was temporized with dextrose infusion and diazoxide and resolved with carboplatin and etoposide. PET-CT two months later revealed a markedly FDG avid 2.2 cm left liver lobe lesion and no pancreatic FDG uptake. A repeat CT five months later showed interval size decrease of the hepatic and pancreatic lesion(s). She currently remains on a 4-week course of durvalumab.
Discussion: Malignant insulinoma should be an etiologic consideration in patients with severe refractory hypoglycemia in the setting of hepatic metastases. Due to the advanced age of our patient and presence of extensive liver metastases, curative surgical resection was infeasible. In such cases, SSA in combination with chemotherapy remains the mainstay treatment to achieve long term remission of hypoglycemia. Given the high morbidity and mortality associated with metastatic insulinoma, future targeted therapeutic strategies should consider the biochemical and genetic mechanisms accounting for its pathogenesis.
Disclosures:
Samier Deen, DO1, Ahmed Abidali, DO2, Jacob T. Harris, MD1, Faisal Mehmood, MD1, Gavin Levinthal, MD1, Bassel Al-Lahham, MD3. P0183 - Refractory Neuroglycopenia and Hyperinsulinemia: An Unusual Case of Metastatic Pancreatic Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HonorHealth, Scottsdale, AZ; 2Abrazo Health, Glendale, AZ; 3HonorHealth, Phoenix, AZ
Introduction: Metastatic insulinoma, a rare form of pancreatic neuroendocrine tumor (panNET), is hypothesized to originate from non-functioning panNETs. Malignant transformation and hepatic metastasis are highly unusual features, accounting for only a fraction of panNET cases. Symptoms are often attributed to refractory hypoglycemia, including confusion, headaches, and diarrhea. Endoscopic ultrasonography (EUS) is a viable diagnostic modality in cases where pancreatic lesions are indiscernible on CT, but suspicion is high. Treatment often includes somatostatin analogues (SSA) and chemotherapy, resulting in resolution of hypoglycemia.
Case Description/Methods: A 70-year-old female with a history of type 2 diabetes mellitus, hypertension and coronary artery disease presented with a 1-day history of confusion, diarrhea, and headaches. Initial labs were remarkable for profound hypokalemia and hypoglycemia (nadir of 30 mg/dL). MRI liver protocol demonstrated numerous hepatic lesions with the largest measuring 8.0 x 7.5 cm in the left liver lobe. EUS revealed a 2.4 x 2.1 cm pancreatic neck mass and left hepatic lobe mass, and biopsies were obtained. Bidirectional endoscopy was unrevealing. Pathology demonstrated poorly differentiated neuroendocrine carcinoma with hepatic metastasis. Immunohistochemical analysis revealed positive staining for INSM1, AE1/AE3, chromogranin, synaptophysin, CD56, Ki-67 index >20%, and antibodies against S-100. CA 19-9, fasting insulin, proinsulin, and c-peptide levels were markedly elevated. Her refractory hypoglycemia was temporized with dextrose infusion and diazoxide and resolved with carboplatin and etoposide. PET-CT two months later revealed a markedly FDG avid 2.2 cm left liver lobe lesion and no pancreatic FDG uptake. A repeat CT five months later showed interval size decrease of the hepatic and pancreatic lesion(s). She currently remains on a 4-week course of durvalumab.
Discussion: Malignant insulinoma should be an etiologic consideration in patients with severe refractory hypoglycemia in the setting of hepatic metastases. Due to the advanced age of our patient and presence of extensive liver metastases, curative surgical resection was infeasible. In such cases, SSA in combination with chemotherapy remains the mainstay treatment to achieve long term remission of hypoglycemia. Given the high morbidity and mortality associated with metastatic insulinoma, future targeted therapeutic strategies should consider the biochemical and genetic mechanisms accounting for its pathogenesis.
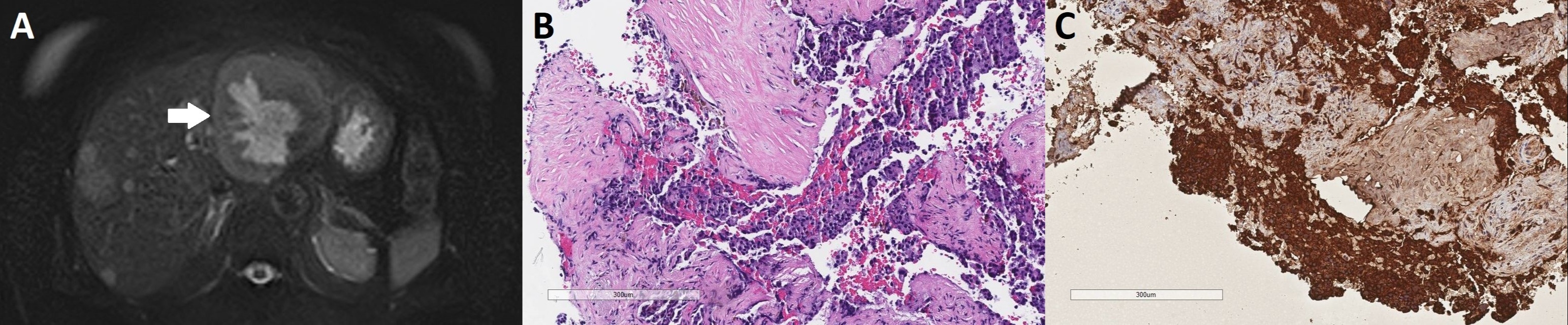
Figure: Figure A: MRI liver protocol demonstrating left hepatic lobe dominant lesion measuring 8.0 x 7.5 cm (arrow).
Figure B: High power field image of H&E stain demonstrating poorly differentiated neuroendocrine carcinoma.
Figure C: High power field image of tumor cells staining positive for chromogranin.
Figure B: High power field image of H&E stain demonstrating poorly differentiated neuroendocrine carcinoma.
Figure C: High power field image of tumor cells staining positive for chromogranin.
Disclosures:
Samier Deen indicated no relevant financial relationships.
Ahmed Abidali indicated no relevant financial relationships.
Jacob Harris indicated no relevant financial relationships.
Faisal Mehmood indicated no relevant financial relationships.
Gavin Levinthal indicated no relevant financial relationships.
Bassel Al-Lahham indicated no relevant financial relationships.
Samier Deen, DO1, Ahmed Abidali, DO2, Jacob T. Harris, MD1, Faisal Mehmood, MD1, Gavin Levinthal, MD1, Bassel Al-Lahham, MD3. P0183 - Refractory Neuroglycopenia and Hyperinsulinemia: An Unusual Case of Metastatic Pancreatic Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
