Sunday Poster Session
Category: Biliary/Pancreas
P0191 - Diagnosis of Non-Functional Pancreatic Neuroendocrine Tumor in a Patient with a Transplanted Pancreas: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- TH
Taraneh Honarparvar, MD
Nova Southeastern University
Wellington, FL
Presenting Author(s)
Taraneh Honarparvar, MD1, Baha Fawwaz, MBBS2, Mohammad M. Asfari, MD2
1Nova Southeastern University, Wellington, FL; 2AdventHealth, Orlando, FL
Introduction: Neuroendocrine tumors (NETs) are rare tumors that can affect pancreas. These are the second most common pancreatic tumors after pancreatic ductal adenocarcinoma (pNETs). The incidence and prevalence of pNETs has been rising secondary to improved detection through imaging. Pancreatic neuroendocrine tumors are primarily sporadic, but can result from genetic mutations. Hereby, we present a case of pNET in a transplanted pancreas.
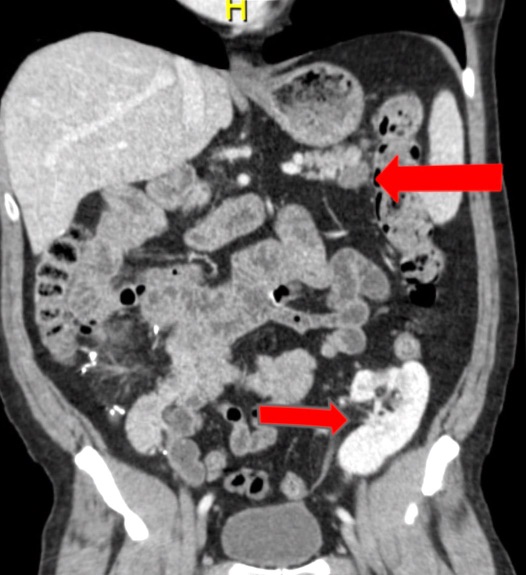
Case Description/Methods: A 51-year-old man with a medical history of diabetes mellitus type II and end-stage renal disease, status post simultaneous kidney and pancreas transplant from a 48-year-old deceased donor, two years before his presentation. The patient presented to clinic with persistent discomfort in the upper abdomen for one year. His post-transplant course was complicated by acute pancreatitis, resulting in walled-off necrosis in the pancreatic tail. After failure of a proton pump inhibitor trial, an upper endoscopy was pursued which was inconclusive. Magnetic resonance cholangiopancreatography revealed a nonenhancing area involving the pancreatic tail. Chromogranin A level was elevated. An endoscopic ultrasound with a fine needle biopsy revealed a low-grade, well-differentiated pNET. The patient underwent a laparoscopic splenic-preserving distal pancreatectomy with intraoperative ultrasound. Histopathology revealed a well-differentiated neuroendocrine neoplasm (0.7 cm), Grade 1, with negative margins and sentinel lymph nodes.
Discussion: Pancreatic neuroendocrine tumors (pNET) have never been reported in a transplanted pancreas. Pancreatic NETs can be either non-functional or functional by secreting hormones. Depending on the primary tumor location, size, and functionality, patients can be asymptomatic or symptomatic. Various imaging techniques used in diagnosing of PNETs such as multiphasic computed tomography (CT), magnetic resonance imaging (MRI), and endoscopic ultrasound with fine needle biopsy. Tumor markers include serum neuron-specific enolase, chromogranin A (CgA), among others. The primary prognostic factor relies on tumor grade and stage. Management of the pNETs depends on the tumor size, functionality, risk of distant metastasis, and the patient’s symptoms and preference. While active surveillance is the preferred approach in non-functional, sporadic, small size PNETs (less than 2 cm) surgery remains the optimal choice in patients with functional tumors. Treatment of NETs should be individualized and involve a multidisciplinary team approach.
Disclosures:
Taraneh Honarparvar, MD1, Baha Fawwaz, MBBS2, Mohammad M. Asfari, MD2. P0191 - Diagnosis of Non-Functional Pancreatic Neuroendocrine Tumor in a Patient with a Transplanted Pancreas: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Nova Southeastern University, Wellington, FL; 2AdventHealth, Orlando, FL
Introduction: Neuroendocrine tumors (NETs) are rare tumors that can affect pancreas. These are the second most common pancreatic tumors after pancreatic ductal adenocarcinoma (pNETs). The incidence and prevalence of pNETs has been rising secondary to improved detection through imaging. Pancreatic neuroendocrine tumors are primarily sporadic, but can result from genetic mutations. Hereby, we present a case of pNET in a transplanted pancreas.
Case Description/Methods: A 51-year-old man with a medical history of diabetes mellitus type II and end-stage renal disease, status post simultaneous kidney and pancreas transplant from a 48-year-old deceased donor, two years before his presentation. The patient presented to clinic with persistent discomfort in the upper abdomen for one year. His post-transplant course was complicated by acute pancreatitis, resulting in walled-off necrosis in the pancreatic tail. After failure of a proton pump inhibitor trial, an upper endoscopy was pursued which was inconclusive. Magnetic resonance cholangiopancreatography revealed a nonenhancing area involving the pancreatic tail. Chromogranin A level was elevated. An endoscopic ultrasound with a fine needle biopsy revealed a low-grade, well-differentiated pNET. The patient underwent a laparoscopic splenic-preserving distal pancreatectomy with intraoperative ultrasound. Histopathology revealed a well-differentiated neuroendocrine neoplasm (0.7 cm), Grade 1, with negative margins and sentinel lymph nodes.
Discussion: Pancreatic neuroendocrine tumors (pNET) have never been reported in a transplanted pancreas. Pancreatic NETs can be either non-functional or functional by secreting hormones. Depending on the primary tumor location, size, and functionality, patients can be asymptomatic or symptomatic. Various imaging techniques used in diagnosing of PNETs such as multiphasic computed tomography (CT), magnetic resonance imaging (MRI), and endoscopic ultrasound with fine needle biopsy. Tumor markers include serum neuron-specific enolase, chromogranin A (CgA), among others. The primary prognostic factor relies on tumor grade and stage. Management of the pNETs depends on the tumor size, functionality, risk of distant metastasis, and the patient’s symptoms and preference. While active surveillance is the preferred approach in non-functional, sporadic, small size PNETs (less than 2 cm) surgery remains the optimal choice in patients with functional tumors. Treatment of NETs should be individualized and involve a multidisciplinary team approach.
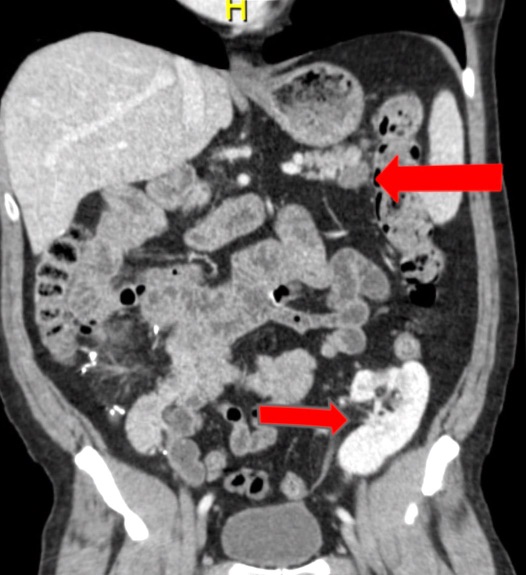
Figure: Figure 1: Abdominal CT with IV contrast coronal view, left arrow: pancreatic tail tumor, right arrow: a transplanted kidney.
Disclosures:
Taraneh Honarparvar indicated no relevant financial relationships.
Baha Fawwaz indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Taraneh Honarparvar, MD1, Baha Fawwaz, MBBS2, Mohammad M. Asfari, MD2. P0191 - Diagnosis of Non-Functional Pancreatic Neuroendocrine Tumor in a Patient with a Transplanted Pancreas: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
