Sunday Poster Session
Category: Biliary/Pancreas
P0108 - Epstein-Barr Virus-Induced Hepatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- ZW
Zainulabedin Waqar, MD
Mercy Medical Center
Toledo, OH
Presenting Author(s)
Zainulabedin Waqar, MD1, Ratika Dogra, MD2, Julie Schira, FNP3, Brandon Wong, MD3
1Mercy Medical Center, Toledo, OH; 2Mercy Hospital, Toledo, OH; 3Mercy Health, Toledo, OH
Introduction: Epstein Barr virus is a double stranded DNA virus that infects a human host and commonly it is an infection of childhood and adolescents primarily as infectious mononucleosis. Many children remain asymptomatic but the disease can become more characteristic in adolescents. Adult infections of Epstein Barr Virus are most commonly described in immunocompromised individuals and known to cause hepatitis and liver cirrhosis. Our case discusses an immunocompetent host that had jaundice secondary to EBV.
Case Description/Methods: 54-year-old female with no past medical history presents with 2 weeks of fever, headaches and congestion. Family had noticed that the patient had become yellow for the past few days. Patient found to have jaundice and elevated bilirubin of 33 mg/dL, Ethanol was negative, Lipase 24, ammonia 33. Hepatitis B surface antigen negative, Hepatitis C Ab nonreactive, Hepatitis B Core IGM nonreactive, Hep A IgM non-reactive, Patient underwent MRCP showing pericholecystic edema without acute cholecystitis and mild hepatosteatosis. Of note, the patient also had anemia. Patient was found to be positive for EBV with IgM 1017 u/mL (Normal range < 100 U/mL). Patient diagnosed with EBV hepatitis causing direct bilirubinemia. On follow up post discharge her liver function continued to improve.
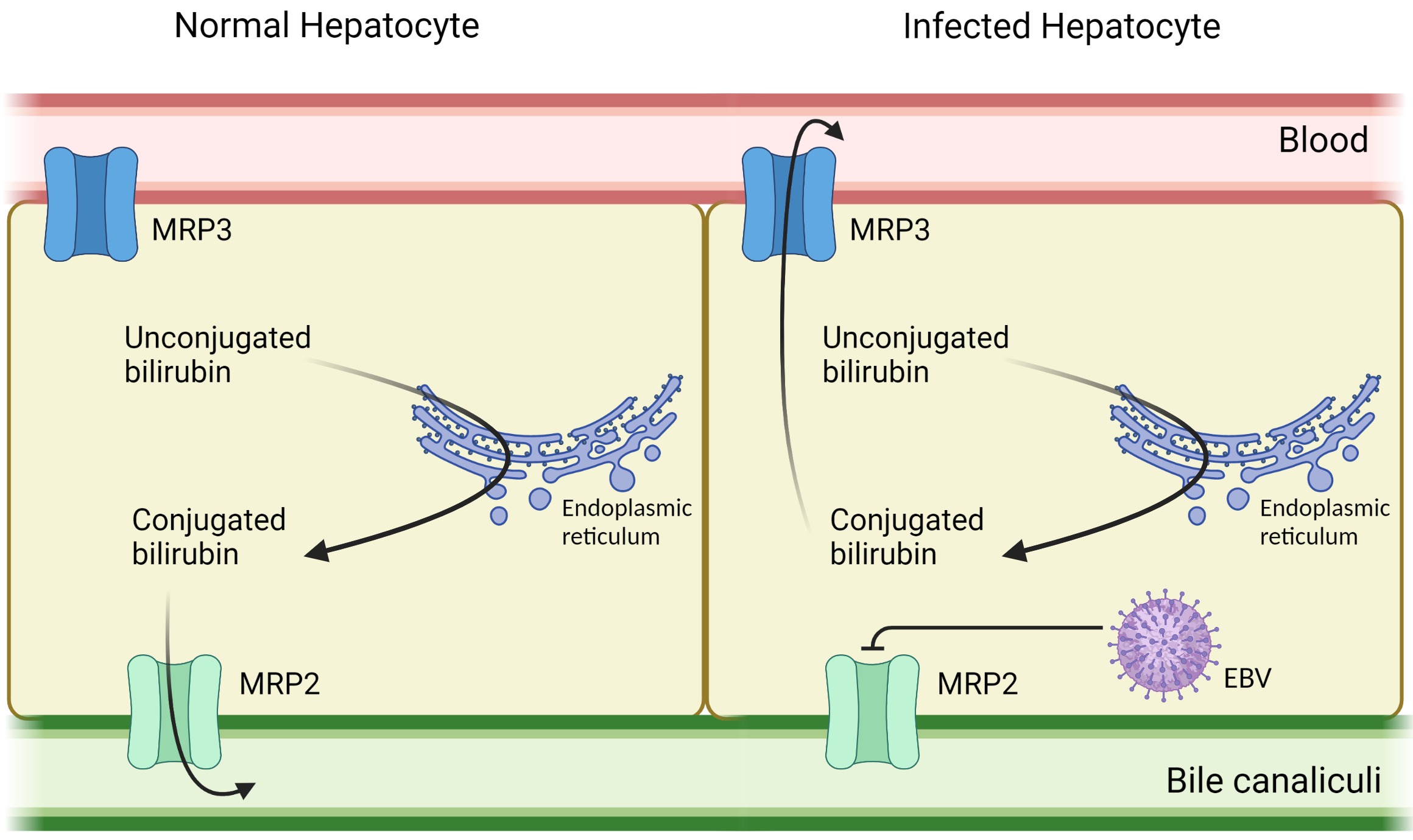
Discussion: Epstein-Barr virus, also known as human herpesvirus 4 is one of the most common human viruses and the primary cause of Infectious mononucleosis. Hepatic involvement is usually characterized by mild elevations of liver enzymes seen in 90% of the patients and self-limited; severe cholestasis with jaundice are uncommon. Complications of EBV infection are believed to be immune mediated rather than cytotoxic and many events can occur because of the host response to the EBV infection of the B-cell. Lymphocytic infiltration of the liver and proliferation of Kupffer cells lead to mild intrahepatic cholestasis but with maintenance of the lobular architecture and without necrosis. Mild, transient elevations in hepatic transaminases are common during the second to fourth weeks of illness. While cholestasis can occur during the convalescent phase of any severe form of viral hepatitis, elevated ALP and bilirubin levels are not typically associated with EBV infection. One of the proposed mechanisms is that EBV inhibits MRP2, which is the main bilirubin transporter (figure 1). Furthermore, high levels of GGT activity were observed, suggesting virus-induced self-limiting cholangiocyte damage
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zainulabedin Waqar, MD1, Ratika Dogra, MD2, Julie Schira, FNP3, Brandon Wong, MD3. P0108 - Epstein-Barr Virus-Induced Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mercy Medical Center, Toledo, OH; 2Mercy Hospital, Toledo, OH; 3Mercy Health, Toledo, OH
Introduction: Epstein Barr virus is a double stranded DNA virus that infects a human host and commonly it is an infection of childhood and adolescents primarily as infectious mononucleosis. Many children remain asymptomatic but the disease can become more characteristic in adolescents. Adult infections of Epstein Barr Virus are most commonly described in immunocompromised individuals and known to cause hepatitis and liver cirrhosis. Our case discusses an immunocompetent host that had jaundice secondary to EBV.
Case Description/Methods: 54-year-old female with no past medical history presents with 2 weeks of fever, headaches and congestion. Family had noticed that the patient had become yellow for the past few days. Patient found to have jaundice and elevated bilirubin of 33 mg/dL, Ethanol was negative, Lipase 24, ammonia 33. Hepatitis B surface antigen negative, Hepatitis C Ab nonreactive, Hepatitis B Core IGM nonreactive, Hep A IgM non-reactive, Patient underwent MRCP showing pericholecystic edema without acute cholecystitis and mild hepatosteatosis. Of note, the patient also had anemia. Patient was found to be positive for EBV with IgM 1017 u/mL (Normal range < 100 U/mL). Patient diagnosed with EBV hepatitis causing direct bilirubinemia. On follow up post discharge her liver function continued to improve.
Discussion: Epstein-Barr virus, also known as human herpesvirus 4 is one of the most common human viruses and the primary cause of Infectious mononucleosis. Hepatic involvement is usually characterized by mild elevations of liver enzymes seen in 90% of the patients and self-limited; severe cholestasis with jaundice are uncommon. Complications of EBV infection are believed to be immune mediated rather than cytotoxic and many events can occur because of the host response to the EBV infection of the B-cell. Lymphocytic infiltration of the liver and proliferation of Kupffer cells lead to mild intrahepatic cholestasis but with maintenance of the lobular architecture and without necrosis. Mild, transient elevations in hepatic transaminases are common during the second to fourth weeks of illness. While cholestasis can occur during the convalescent phase of any severe form of viral hepatitis, elevated ALP and bilirubin levels are not typically associated with EBV infection. One of the proposed mechanisms is that EBV inhibits MRP2, which is the main bilirubin transporter (figure 1). Furthermore, high levels of GGT activity were observed, suggesting virus-induced self-limiting cholangiocyte damage
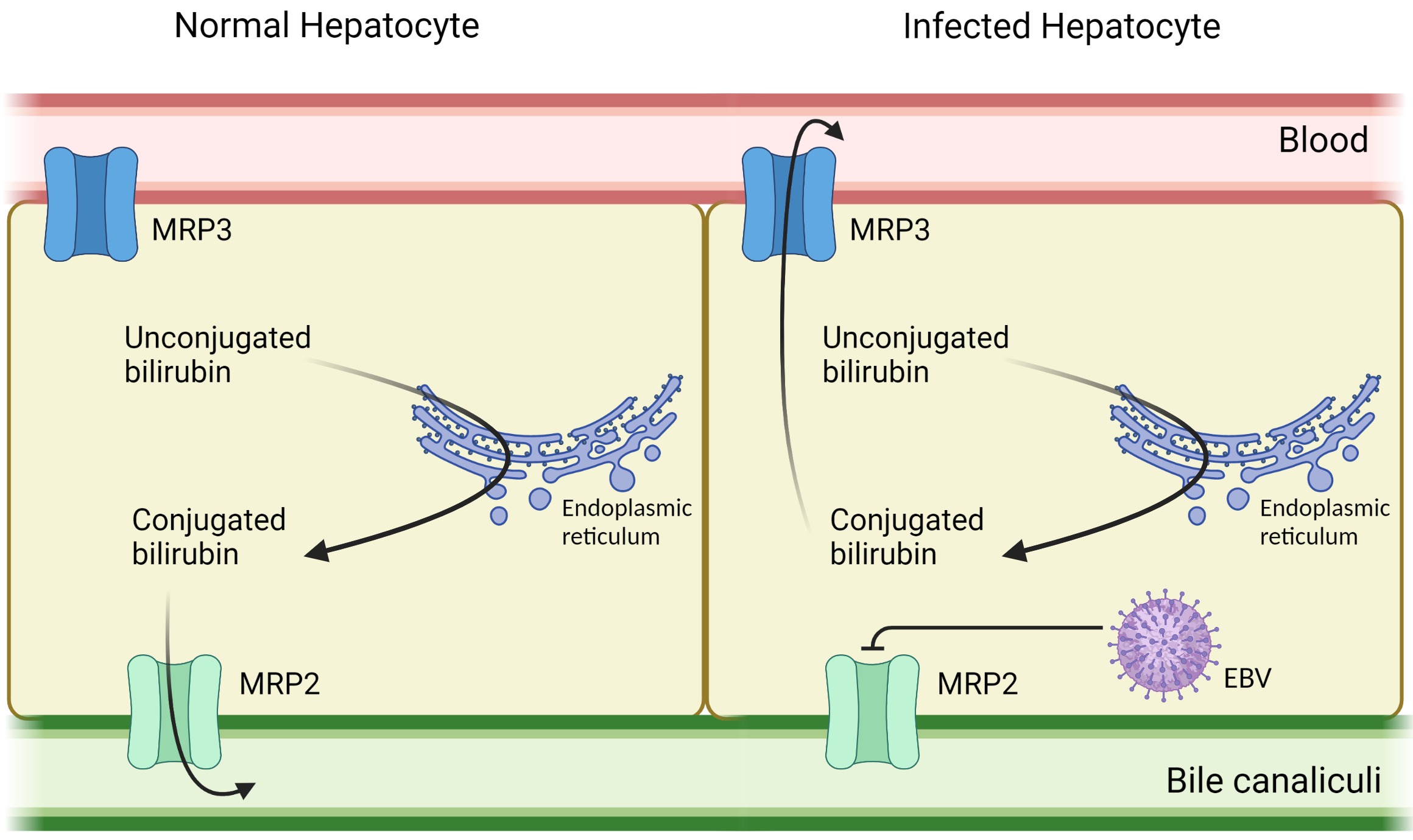
Figure: Proposed mechanism of EBV infection
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zainulabedin Waqar indicated no relevant financial relationships.
Ratika Dogra indicated no relevant financial relationships.
Julie Schira indicated no relevant financial relationships.
Brandon Wong indicated no relevant financial relationships.
Zainulabedin Waqar, MD1, Ratika Dogra, MD2, Julie Schira, FNP3, Brandon Wong, MD3. P0108 - Epstein-Barr Virus-Induced Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
