Sunday Poster Session
Category: Biliary/Pancreas
P0109 - Chronic Pancreatitis Secondary to Semaglutide Use
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Charles Vallejo, DO
Florida Atlantic University
Boca Raton, FL
Presenting Author(s)
Charles Vallejo, DO1, Ritu Channagiri, BS2, Spencer Barnes, BS3, Kevin Vallejo, MD4, Roozbeh Nazarian, MD3
1Florida Atlantic University, Boca Raton, FL; 2Cleveland Clinic Florida, Boca Raton, FL; 3Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL; 4HCA Florida Healthcare, Miami, FL
Introduction: Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) which is an injectable glucose-lowering pharmaceutical used to treat type II diabetes mellitus (DM2) and is one of the most efficacious glucose-lowering agents available today. GLP-1 RAs bind pancreatic beta cells to stimulate insulin secretion as well as stimulate insulin synthesis at the translational level. Other mechanisms include decreased endogenous glucose production and delayed gastric emptying. Potential adverse effects of GLP-1 RAs include acute pancreatitis, medullary thyroid carcinoma, and nonspecific gastrointestinal symptoms. We present a case of chronic pancreatitis induced by prolonged usage of semaglutide.
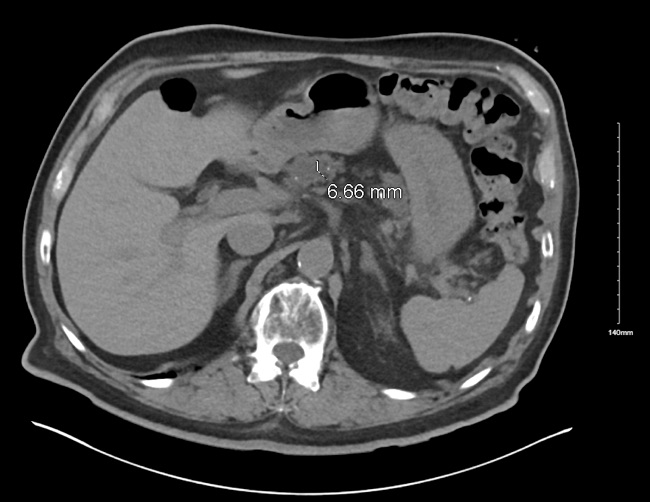
Case Description/Methods: A 79-year-old male with a history of chronic kidney disease, hypertension, DM2 on semaglutide 1mg for the past 2.5 years presented due to profuse watery diarrhea for the past 2 months. He admitted to an unintentional weight loss of 20 lbs over the last 2 months. He endorsed low-grade abdominal pain for the past year. He presented with a creatinine 5.2, up from his baseline of 2. The patient was found to have acute tubular necrosis due to chronic hypoperfusion secondary to GI losses. Labs were remarkable for a lipase of 584. CT abdomen without contrast revealed coarse calcifications seen throughout the pancreas concerning for chronic pancreatitis with dilation of the main pancreatic duct up to 7mm. Fecal elastase was found to be 44 ug/g consistent with severe pancreatic insufficiency. The patient was suspected to have chronic pancreatitis secondary to GLP-1 RA use. Semaglutide was discontinued, and he was started on pancrelipase with resolution of his diarrhea.
Discussion: GLP-1 RAs have been associated with an increased risk of pancreatitis and pancreatic cancer in diabetic patients. Patients with pancreatitis are not recommended to continue GLP-1 RAs and switch to a different antidiabetic therapy class. Since GLP-1 RAs are expressed by pancreatic islet and exocrine duct cells, repeated stimulation of these receptors may lead to overgrowth of the cells that the small ducts, resulting in surrounding hyperplasia and a state of chronic inflammation. This patient likely experienced chronic pancreatitis due to prolonged semaglutide use, as evidenced by his clinical course and resolution of symptoms upon initiation of pancrelipase. Clinicians must understand the potential adverse effects that may be induced by GLP-1 RAs as their popularity and usage continues to increase.
Disclosures:
Charles Vallejo, DO1, Ritu Channagiri, BS2, Spencer Barnes, BS3, Kevin Vallejo, MD4, Roozbeh Nazarian, MD3. P0109 - Chronic Pancreatitis Secondary to Semaglutide Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Florida Atlantic University, Boca Raton, FL; 2Cleveland Clinic Florida, Boca Raton, FL; 3Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL; 4HCA Florida Healthcare, Miami, FL
Introduction: Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) which is an injectable glucose-lowering pharmaceutical used to treat type II diabetes mellitus (DM2) and is one of the most efficacious glucose-lowering agents available today. GLP-1 RAs bind pancreatic beta cells to stimulate insulin secretion as well as stimulate insulin synthesis at the translational level. Other mechanisms include decreased endogenous glucose production and delayed gastric emptying. Potential adverse effects of GLP-1 RAs include acute pancreatitis, medullary thyroid carcinoma, and nonspecific gastrointestinal symptoms. We present a case of chronic pancreatitis induced by prolonged usage of semaglutide.
Case Description/Methods: A 79-year-old male with a history of chronic kidney disease, hypertension, DM2 on semaglutide 1mg for the past 2.5 years presented due to profuse watery diarrhea for the past 2 months. He admitted to an unintentional weight loss of 20 lbs over the last 2 months. He endorsed low-grade abdominal pain for the past year. He presented with a creatinine 5.2, up from his baseline of 2. The patient was found to have acute tubular necrosis due to chronic hypoperfusion secondary to GI losses. Labs were remarkable for a lipase of 584. CT abdomen without contrast revealed coarse calcifications seen throughout the pancreas concerning for chronic pancreatitis with dilation of the main pancreatic duct up to 7mm. Fecal elastase was found to be 44 ug/g consistent with severe pancreatic insufficiency. The patient was suspected to have chronic pancreatitis secondary to GLP-1 RA use. Semaglutide was discontinued, and he was started on pancrelipase with resolution of his diarrhea.
Discussion: GLP-1 RAs have been associated with an increased risk of pancreatitis and pancreatic cancer in diabetic patients. Patients with pancreatitis are not recommended to continue GLP-1 RAs and switch to a different antidiabetic therapy class. Since GLP-1 RAs are expressed by pancreatic islet and exocrine duct cells, repeated stimulation of these receptors may lead to overgrowth of the cells that the small ducts, resulting in surrounding hyperplasia and a state of chronic inflammation. This patient likely experienced chronic pancreatitis due to prolonged semaglutide use, as evidenced by his clinical course and resolution of symptoms upon initiation of pancrelipase. Clinicians must understand the potential adverse effects that may be induced by GLP-1 RAs as their popularity and usage continues to increase.
Figure: Figure 1: Abdominal CT demonstrating pancreatic ductal dilation and calcifications
Disclosures:
Charles Vallejo indicated no relevant financial relationships.
Ritu Channagiri indicated no relevant financial relationships.
Spencer Barnes indicated no relevant financial relationships.
Kevin Vallejo indicated no relevant financial relationships.
Roozbeh Nazarian indicated no relevant financial relationships.
Charles Vallejo, DO1, Ritu Channagiri, BS2, Spencer Barnes, BS3, Kevin Vallejo, MD4, Roozbeh Nazarian, MD3. P0109 - Chronic Pancreatitis Secondary to Semaglutide Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
