Sunday Poster Session
Category: Biliary/Pancreas
P0113 - A Rare Case of Metastatic Insulinoma With Benign Features on Imaging
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Cynthia Edimo, DO
Stony Brook University Hospital
Stony Brook, NY
Presenting Author(s)
Cynthia Edimo, DO, Adam Slavick, MD, Artemio Zavala, MD, Leslie Klyachman, MD
Stony Brook University Hospital, Stony Brook, NY
Introduction: Insulinomas are rare pancreatic neuroendocrine tumors that secrete insulin regardless of blood glucose levels. We present a case of a metastatic insulinoma that appeared benign on imaging.
Case Description/Methods: A 49 year-old female with a past medical history of breast cancer status-post core lumpectomy in 2021 on tamoxifen, and thyroid nodules presented with complaints of “brain fog” and tremors, associated with fasting. The symptoms recently worsened after the patient started a low carbohydrate diet. Lab work was significant for a glucose fingerstick of 93, and after 1.5 hours, a fingerstick of 61. The patient then underwent a 72-hour fast. Two hours into the fast, labs showed a blood glucose of 53, insulin level of 19 uIU/mL, C-peptide of 6.2 ng/mL and intact pro-insulin of 5.5 pmol/L. Sulfonylurea screen was negative. MRI was obtained with findings of a cystic lesion in the pancreatic head, without worrisome features, suggestive of a side branch intraductal papillary mucinous neoplasm (IPMN). An endoscopic ultrasound with biopsy was performed and samples of the pancreatic head and a lymph node at the gastrohepatic ligament were obtained. Pathology for both was positive for atypical cells suggestive of a neuroendocrine tumor. The patient was discharged and followed up with a dotatate PET/CT scan which was consistent with receptor expressing neuroendocrine tumor of the pancreatic head and a metastatic node in the gastrohepatic region. MEN-1 gene testing was negative. The patient underwent a Whipple procedure 5 weeks later.
Discussion: Our patient was diagnosed with a malignant insulinoma, despite MRI imaging that was suggestive of a side-branch IPMN. Branch-duct lesions are typically lower risk for malignancy in comparison to main duct lesions. Concerning findings of IPMNs include size greater than 30 mm, thickened or enhancing cyst walls, dilated main pancreatic duct, or associated pancreatitis1. Our patient’s cystic lesion was described as a 10 x 16 x 9 mm non-enhancing lesion without a thick capsule, which deviated from the typical concerning characteristics seen on MRI. While imaging plays a crucial role, this case emphasizes the potential limitations of imaging data for diagnosis, underscoring the importance of clinical suspicion.
References:
1. Kim KW, Park SH, Pyo J, et al. Imaging features to distinguish malignant and benign branch-duct type intraductal papillary mucinous neoplasms of the pancreas. Annals of Surgery. 2014 Jan;259(1):72–81. doi:10.1097/sla.0b013e31829385f7
Disclosures:
Cynthia Edimo, DO, Adam Slavick, MD, Artemio Zavala, MD, Leslie Klyachman, MD. P0113 - A Rare Case of Metastatic Insulinoma With Benign Features on Imaging, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Stony Brook University Hospital, Stony Brook, NY
Introduction: Insulinomas are rare pancreatic neuroendocrine tumors that secrete insulin regardless of blood glucose levels. We present a case of a metastatic insulinoma that appeared benign on imaging.
Case Description/Methods: A 49 year-old female with a past medical history of breast cancer status-post core lumpectomy in 2021 on tamoxifen, and thyroid nodules presented with complaints of “brain fog” and tremors, associated with fasting. The symptoms recently worsened after the patient started a low carbohydrate diet. Lab work was significant for a glucose fingerstick of 93, and after 1.5 hours, a fingerstick of 61. The patient then underwent a 72-hour fast. Two hours into the fast, labs showed a blood glucose of 53, insulin level of 19 uIU/mL, C-peptide of 6.2 ng/mL and intact pro-insulin of 5.5 pmol/L. Sulfonylurea screen was negative. MRI was obtained with findings of a cystic lesion in the pancreatic head, without worrisome features, suggestive of a side branch intraductal papillary mucinous neoplasm (IPMN). An endoscopic ultrasound with biopsy was performed and samples of the pancreatic head and a lymph node at the gastrohepatic ligament were obtained. Pathology for both was positive for atypical cells suggestive of a neuroendocrine tumor. The patient was discharged and followed up with a dotatate PET/CT scan which was consistent with receptor expressing neuroendocrine tumor of the pancreatic head and a metastatic node in the gastrohepatic region. MEN-1 gene testing was negative. The patient underwent a Whipple procedure 5 weeks later.
Discussion: Our patient was diagnosed with a malignant insulinoma, despite MRI imaging that was suggestive of a side-branch IPMN. Branch-duct lesions are typically lower risk for malignancy in comparison to main duct lesions. Concerning findings of IPMNs include size greater than 30 mm, thickened or enhancing cyst walls, dilated main pancreatic duct, or associated pancreatitis1. Our patient’s cystic lesion was described as a 10 x 16 x 9 mm non-enhancing lesion without a thick capsule, which deviated from the typical concerning characteristics seen on MRI. While imaging plays a crucial role, this case emphasizes the potential limitations of imaging data for diagnosis, underscoring the importance of clinical suspicion.
References:
1. Kim KW, Park SH, Pyo J, et al. Imaging features to distinguish malignant and benign branch-duct type intraductal papillary mucinous neoplasms of the pancreas. Annals of Surgery. 2014 Jan;259(1):72–81. doi:10.1097/sla.0b013e31829385f7
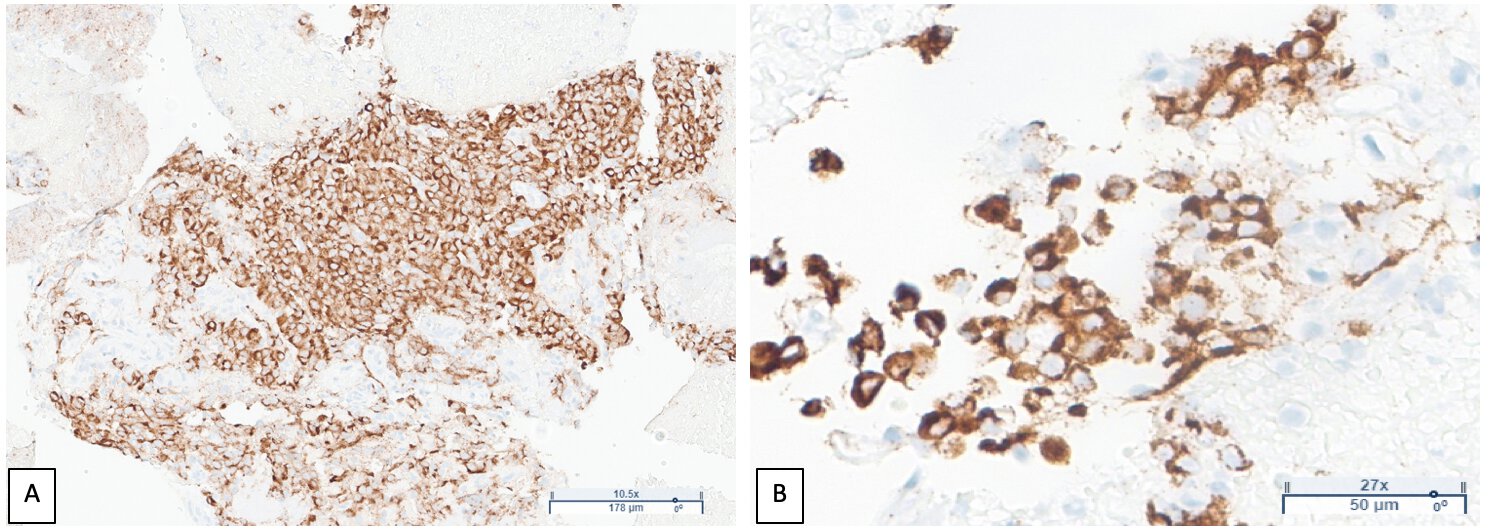
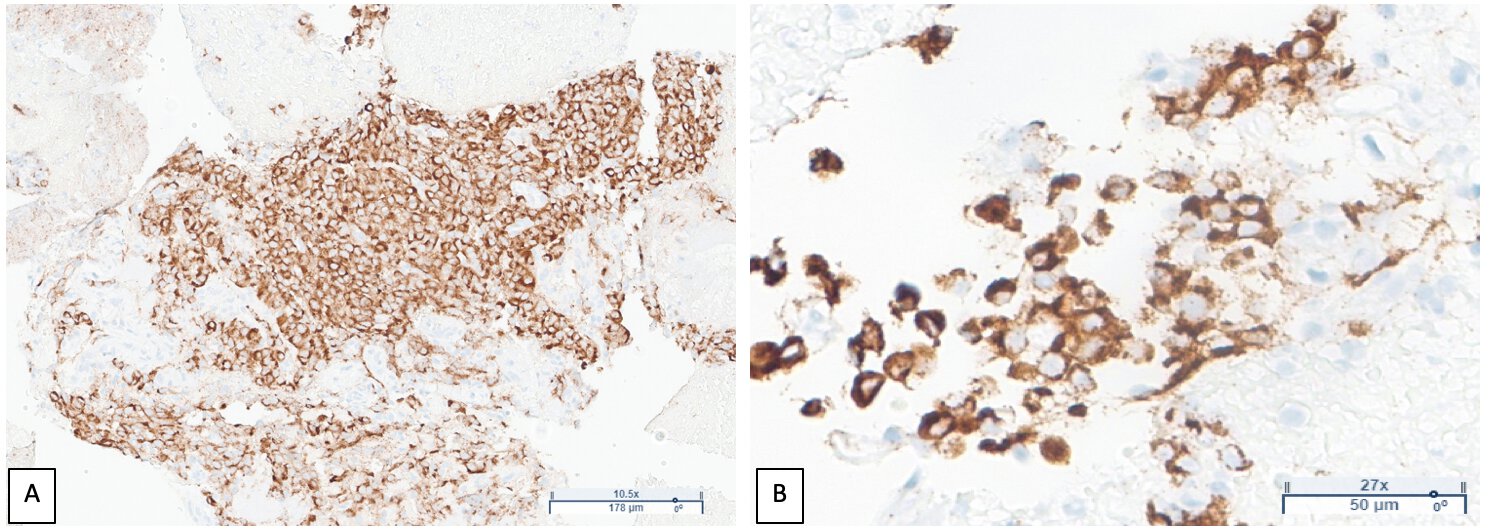
Figure: A. Fine needle aspiration of a gastrohepatic ligament lymph node demonstrating strongly positive immunostain for chromogranin, consistent with neuroendocrine differentiation.
B. Fine needle aspiration of the pancreatic mass demonstrating strongly positive immunostain for chromogranin, consistent with neuroendocrine differentiation.
B. Fine needle aspiration of the pancreatic mass demonstrating strongly positive immunostain for chromogranin, consistent with neuroendocrine differentiation.
Disclosures:
Cynthia Edimo indicated no relevant financial relationships.
Adam Slavick indicated no relevant financial relationships.
Artemio Zavala indicated no relevant financial relationships.
Leslie Klyachman indicated no relevant financial relationships.
Cynthia Edimo, DO, Adam Slavick, MD, Artemio Zavala, MD, Leslie Klyachman, MD. P0113 - A Rare Case of Metastatic Insulinoma With Benign Features on Imaging, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
