Sunday Poster Session
Category: Biliary/Pancreas
P0119 - Right Atrial Thrombus Induced by Pancreatic Pseudocyst
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Salim C. Lutfallah, BS
LSU Health New Orleans School of Medicine
Metairie, LA
Presenting Author(s)
Salim C.. Lutfallah, BS1, Brooke McVaney, DO2, Catherine Loehr, MD3, Jorge Martinez, MD, JD3
1LSU Health New Orleans School of Medicine, Metairie, LA; 2LSU Health New Orleans School of Medicine, New Orleans, LA; 3LSU, New Orleans, LA
Introduction: Thrombus formation in the context of pancreatitis is an infrequent condition, with pancreatic pseudocyst-associated thrombosis being an even rarer phenomena documented in the literature. Here we present a patient case of chronic pancreatitis complicated by the presence of a pancreatic pseudocyst. This patient exhibited no conventional thrombogenic risk factors, yet subsequently developed a thrombus in the right atrium.
Case Description/Methods: A 45-year-old woman, with a medical history significant for chronic alcohol use, chronic pancreatitis, biliary stricture, and unintentional weight loss of 70lbs, presented due to concerns of esophageal perforation after undergoing an endoscopic retrograde cholangiopancreatography 3 days earlier.
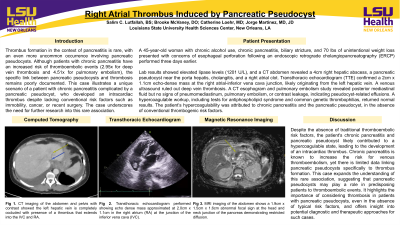
Laboratory findings showed elevated lipase levels at 1201 U/L, while a computed tomography (CT) abdomen uncovered a 4 cm right hepatic abscess, pancreatic pseudocyst with enhancement near porta hepatis, cholangitis, and a right atrial clot. Transesophageal echocardiography (TTE) confirmed the presence of an echo-dense mass measuring 2cm x 1.1cm in the right atrial-inferior vena cava junction, likely originating from the left hepatic vein and extending into the right atrium. Duplex venous leg ultrasound ruled out deep vein thrombosis. A CT esophogram and CT pulmonary embolism study revealed posterior mediastinal fluid but no pneumomediastinum, pulmonary embolisms, or contrast extravasation, indicating pseudocyst-related effusions.
Left thoracentesis yielded 500 mL of exudative, amber-colored fluid; analysis showed 3800 white blood cells/μL with a neutrophilic predominance, 6900 red blood cells/μL, 100 mg/dL glucose, 773 U/L amylase, and 316 U/L lactate dehydrogenase.
Hypercoagulable workup was initiated, with results within normal ranges for the antiphospholipid panel, G20210A mutation, Protein S Antigen, Factor V Leiden, Protein C Antigen, and Factor 2 Assay. With no conventional thrombogenic risk factors identified, the patient’s hypercoagulability was attributed to chronic pancreatitis and the pancreatic pseudocyst.
Discussion: The clinical presentation of this patient, along with the TTE findings and CT results, established the diagnosis of intracardiac thrombus. Predominant risk factors for venous thromboembolism include recent surgical procedures, immobility, cancer, and trauma. This case presents a rare correlation between pancreatic pseudocyst and intracardiac thrombus, without manifestations conventional risk factors or comorbidities.
Disclosures:
Salim C.. Lutfallah, BS1, Brooke McVaney, DO2, Catherine Loehr, MD3, Jorge Martinez, MD, JD3. P0119 - Right Atrial Thrombus Induced by Pancreatic Pseudocyst, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1LSU Health New Orleans School of Medicine, Metairie, LA; 2LSU Health New Orleans School of Medicine, New Orleans, LA; 3LSU, New Orleans, LA
Introduction: Thrombus formation in the context of pancreatitis is an infrequent condition, with pancreatic pseudocyst-associated thrombosis being an even rarer phenomena documented in the literature. Here we present a patient case of chronic pancreatitis complicated by the presence of a pancreatic pseudocyst. This patient exhibited no conventional thrombogenic risk factors, yet subsequently developed a thrombus in the right atrium.
Case Description/Methods: A 45-year-old woman, with a medical history significant for chronic alcohol use, chronic pancreatitis, biliary stricture, and unintentional weight loss of 70lbs, presented due to concerns of esophageal perforation after undergoing an endoscopic retrograde cholangiopancreatography 3 days earlier.
Laboratory findings showed elevated lipase levels at 1201 U/L, while a computed tomography (CT) abdomen uncovered a 4 cm right hepatic abscess, pancreatic pseudocyst with enhancement near porta hepatis, cholangitis, and a right atrial clot. Transesophageal echocardiography (TTE) confirmed the presence of an echo-dense mass measuring 2cm x 1.1cm in the right atrial-inferior vena cava junction, likely originating from the left hepatic vein and extending into the right atrium. Duplex venous leg ultrasound ruled out deep vein thrombosis. A CT esophogram and CT pulmonary embolism study revealed posterior mediastinal fluid but no pneumomediastinum, pulmonary embolisms, or contrast extravasation, indicating pseudocyst-related effusions.
Left thoracentesis yielded 500 mL of exudative, amber-colored fluid; analysis showed 3800 white blood cells/μL with a neutrophilic predominance, 6900 red blood cells/μL, 100 mg/dL glucose, 773 U/L amylase, and 316 U/L lactate dehydrogenase.
Hypercoagulable workup was initiated, with results within normal ranges for the antiphospholipid panel, G20210A mutation, Protein S Antigen, Factor V Leiden, Protein C Antigen, and Factor 2 Assay. With no conventional thrombogenic risk factors identified, the patient’s hypercoagulability was attributed to chronic pancreatitis and the pancreatic pseudocyst.
Discussion: The clinical presentation of this patient, along with the TTE findings and CT results, established the diagnosis of intracardiac thrombus. Predominant risk factors for venous thromboembolism include recent surgical procedures, immobility, cancer, and trauma. This case presents a rare correlation between pancreatic pseudocyst and intracardiac thrombus, without manifestations conventional risk factors or comorbidities.
Disclosures:
Salim Lutfallah indicated no relevant financial relationships.
Brooke McVaney indicated no relevant financial relationships.
Catherine Loehr indicated no relevant financial relationships.
Jorge Martinez indicated no relevant financial relationships.
Salim C.. Lutfallah, BS1, Brooke McVaney, DO2, Catherine Loehr, MD3, Jorge Martinez, MD, JD3. P0119 - Right Atrial Thrombus Induced by Pancreatic Pseudocyst, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
