Sunday Poster Session
Category: Biliary/Pancreas
P0120 - A Rare Case of Immune Checkpoint Cholangitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
- BS
Bipneet Singh, MD
Henry Ford Jackson Hospital
Jackson, MI
Presenting Author(s)
Award: Presidential Poster Award
Bipneet Singh, MD1, Palak Patel-Rodrigues, MD2, Muhammad Zarrar Khan, MD3, Gurleen Kaur, MD4, Sakshi Bai, MD1, Merritt Bern, MD1, Syed-Mohammed Jafri, MD2
1Henry Ford Jackson Hospital, Jackson, MI; 2Henry Ford Health, Detroit, MI; 3Henry Ford Hospital, Royal Oak, MI; 4Government Medical College and Hospital, Khanna, Punjab, India
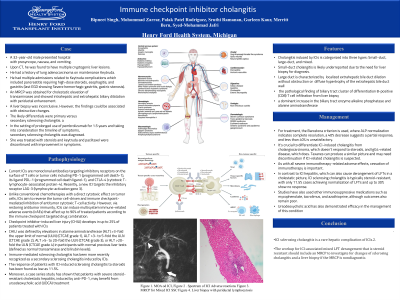
Introduction: Immune checkpoint inhibitor cholangitis (IMC) due to its rarity poses difficulties in diagnosis and treatment. IMC includes a range of biliary tract injuries with different clinical and pathological characteristics, from small-duct to large-duct involvement.
Case Description/Methods: A 32-year-old male presented hospital with presyncope, nausea , and vomiting. Upon CT, he was found to have multiple cryptogenic liver lesions. He had a history of lung adenocarcinoma on maintenance Keytruda. He had multiple admissions related to Keytruda complications which included pancreatitis requiring high-dose steroids, esophagitis, and gastritis (last EGD showing Severe hemorrhagic gastritis, gastric stenosis). An MRCP was obtained for cholestatic elevation of transaminases and showed intrahepatic and extrahepatic biliary dilatation with periductal enhancement. A liver biopsy was inconclusive. However, the findings could be associated with obstructive changes. The likely differentials were primary versus secondary sclerosing cholangitis. In the setting of prolonged use of pembrolizumab for 1.5 years and taking into consideration the timeline of symptoms, secondary sclerosing cholangitis was diagnosed. She was treated with steroids and keytruda and paclitaxel were discontinued with improvement in symptoms.
Discussion: Immune checkpoint inhibitors(ICI) can affect any organ system, including the liver, causing cholangitis, although this is less common than immune-mediated hepatitis. Cholangitis induced by ICIs is categorized into three types: small-duct, large-duct, and mixed. Small-duct cholangitis is likely underreported due to the need for liver biopsy for diagnosis. Its pathology includes bile duct loss, minor bile duct injuries, and mixed inflammatory cells, predominantly CD8+ T cells, diffuse fibrosis in the extrahepatic bile duct with imaging showing nonobstructive dilatation or stenosis. For treatment, the Barcelona criterion is used, where ALP normalization indicates complete resolution, a 40% decrease suggests a partial response, and less than 40% is unsatisfactory. Steroids alone or with immunosuppression show similar results. It's crucial to differentiate ICI-induced cholangitis from cholangiocarcinoma, which doesn't respond to steroids, and IgG4-related disease, which does. Taxanes can produce a similar picture and may need discontinuation if ICI-related cholangitis is suspected.
Disclosures:
Bipneet Singh, MD1, Palak Patel-Rodrigues, MD2, Muhammad Zarrar Khan, MD3, Gurleen Kaur, MD4, Sakshi Bai, MD1, Merritt Bern, MD1, Syed-Mohammed Jafri, MD2. P0120 - A Rare Case of Immune Checkpoint Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Bipneet Singh, MD1, Palak Patel-Rodrigues, MD2, Muhammad Zarrar Khan, MD3, Gurleen Kaur, MD4, Sakshi Bai, MD1, Merritt Bern, MD1, Syed-Mohammed Jafri, MD2
1Henry Ford Jackson Hospital, Jackson, MI; 2Henry Ford Health, Detroit, MI; 3Henry Ford Hospital, Royal Oak, MI; 4Government Medical College and Hospital, Khanna, Punjab, India
Introduction: Immune checkpoint inhibitor cholangitis (IMC) due to its rarity poses difficulties in diagnosis and treatment. IMC includes a range of biliary tract injuries with different clinical and pathological characteristics, from small-duct to large-duct involvement.
Case Description/Methods: A 32-year-old male presented hospital with presyncope, nausea , and vomiting. Upon CT, he was found to have multiple cryptogenic liver lesions. He had a history of lung adenocarcinoma on maintenance Keytruda. He had multiple admissions related to Keytruda complications which included pancreatitis requiring high-dose steroids, esophagitis, and gastritis (last EGD showing Severe hemorrhagic gastritis, gastric stenosis). An MRCP was obtained for cholestatic elevation of transaminases and showed intrahepatic and extrahepatic biliary dilatation with periductal enhancement. A liver biopsy was inconclusive. However, the findings could be associated with obstructive changes. The likely differentials were primary versus secondary sclerosing cholangitis. In the setting of prolonged use of pembrolizumab for 1.5 years and taking into consideration the timeline of symptoms, secondary sclerosing cholangitis was diagnosed. She was treated with steroids and keytruda and paclitaxel were discontinued with improvement in symptoms.
Discussion: Immune checkpoint inhibitors(ICI) can affect any organ system, including the liver, causing cholangitis, although this is less common than immune-mediated hepatitis. Cholangitis induced by ICIs is categorized into three types: small-duct, large-duct, and mixed. Small-duct cholangitis is likely underreported due to the need for liver biopsy for diagnosis. Its pathology includes bile duct loss, minor bile duct injuries, and mixed inflammatory cells, predominantly CD8+ T cells, diffuse fibrosis in the extrahepatic bile duct with imaging showing nonobstructive dilatation or stenosis. For treatment, the Barcelona criterion is used, where ALP normalization indicates complete resolution, a 40% decrease suggests a partial response, and less than 40% is unsatisfactory. Steroids alone or with immunosuppression show similar results. It's crucial to differentiate ICI-induced cholangitis from cholangiocarcinoma, which doesn't respond to steroids, and IgG4-related disease, which does. Taxanes can produce a similar picture and may need discontinuation if ICI-related cholangitis is suspected.
Disclosures:
Bipneet Singh indicated no relevant financial relationships.
Palak Patel-Rodrigues indicated no relevant financial relationships.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Sakshi Bai indicated no relevant financial relationships.
Merritt Bern indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie, Intercept, VectivBio – Advisor or Review Panel Member, Speakers Bureau.
Bipneet Singh, MD1, Palak Patel-Rodrigues, MD2, Muhammad Zarrar Khan, MD3, Gurleen Kaur, MD4, Sakshi Bai, MD1, Merritt Bern, MD1, Syed-Mohammed Jafri, MD2. P0120 - A Rare Case of Immune Checkpoint Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

