Sunday Poster Session
Category: Biliary/Pancreas
P0121 - There is Some Dump in the Sump
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
- BS
Bipneet Singh, MD
Henry Ford Jackson Hospital
Jackson, MI
Presenting Author(s)
Bipneet Singh, MD1, Patrick Lazarczyk, DO2, Sruthi Ramanan, MD1, Gurleen Kaur, MD3, Jahnavi Ethakota, MD1, Merritt Bern, MD1, Roberto Gamarra, MD4
1Henry Ford Jackson Hospital, Jackson, MI; 2Ascension Providence Hospital, Southfield, MI; 3Government Medical College and Hospital, Khanna, Punjab, India; 4Ascension Providence Hospital, Jackson, MI
Introduction: Sump syndrome is a long-term complication of choledochoduodenostomy for biliary drainage in the setting of stones or strictures in days before ERCP was common. Symptoms of cholangitis, 5-10 years after the initial procedure, lead to the suspicion of sump syndrome. ERCP acts both diagnostic and therapeutic with debris removal, and/or stenting and/or sphincterotomy.
Case Description/Methods: 62-year-old male with pancreatic cancer post gastrojejunostomy and cholecystojejunostomy followed by chemo-induced remission 12 years ago presented with nausea, vomiting, and right-sided flank pain. He had been presenting with similar presentations over the past year leading to multiple ERCPs. Upon the last 2 ERCPs, the patient was found to have multiple gall stones in the stump of the common bile duct draining into the duodenum treated with biliary stents. Upon admission, the patient was afebrile with normal vitals and LFTs. Imaging showed a patent stent in the common bile duct. Given his recent history of cholangitis and choledocholithiasis in the common bile duct stump, requiring ERCP-guided stenting, a diagnosis of Sump syndrome was made with the patient developing biliary stasis in the stump causing recurrent obstruction and subclinical infections. General surgery was brought on board to explore the possibility of a Whipple’s procedure versus hepaticojejunostomy to completely resect the frequently affected region altogether.
Discussion: Pre-ERCP, treatment for choledocholithiasis included anastomosis between the common hepatic duct or proximal common bile duct and duodenum with a distal stump draining into the ampulla of Vater. Following the surgery air in the biliary tree acted as the sole indication of functional anastomosis. However, 5-10 years after the procedure, these patients sometimes presented with ascending cholangitis. This phenomenon of the development of stones and subclinical or clinical infection is known as Sump syndrome. The distal duct draining into the ampulla of Vater acts as a recess where static bile and debris keep accumulating, acting as a home for bacterial proliferation. This generally leads to pancreatitis or recurrent cholangitis. For imaging, an ultrasonogram may reveal stones and ductal dilation which might hint at the diagnosis. Finally, ERCP is both diagnostic and therapeutic with sphincterotomy and endoscopic removal. Adequate antibiotic coverage is necessary. Surgical Roux-en-y hepaticojejunostomy proves to be a definitive treatment if the patient requires multiple ERCPs.

Disclosures:
Bipneet Singh, MD1, Patrick Lazarczyk, DO2, Sruthi Ramanan, MD1, Gurleen Kaur, MD3, Jahnavi Ethakota, MD1, Merritt Bern, MD1, Roberto Gamarra, MD4. P0121 - There is Some Dump in the Sump, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Jackson Hospital, Jackson, MI; 2Ascension Providence Hospital, Southfield, MI; 3Government Medical College and Hospital, Khanna, Punjab, India; 4Ascension Providence Hospital, Jackson, MI
Introduction: Sump syndrome is a long-term complication of choledochoduodenostomy for biliary drainage in the setting of stones or strictures in days before ERCP was common. Symptoms of cholangitis, 5-10 years after the initial procedure, lead to the suspicion of sump syndrome. ERCP acts both diagnostic and therapeutic with debris removal, and/or stenting and/or sphincterotomy.
Case Description/Methods: 62-year-old male with pancreatic cancer post gastrojejunostomy and cholecystojejunostomy followed by chemo-induced remission 12 years ago presented with nausea, vomiting, and right-sided flank pain. He had been presenting with similar presentations over the past year leading to multiple ERCPs. Upon the last 2 ERCPs, the patient was found to have multiple gall stones in the stump of the common bile duct draining into the duodenum treated with biliary stents. Upon admission, the patient was afebrile with normal vitals and LFTs. Imaging showed a patent stent in the common bile duct. Given his recent history of cholangitis and choledocholithiasis in the common bile duct stump, requiring ERCP-guided stenting, a diagnosis of Sump syndrome was made with the patient developing biliary stasis in the stump causing recurrent obstruction and subclinical infections. General surgery was brought on board to explore the possibility of a Whipple’s procedure versus hepaticojejunostomy to completely resect the frequently affected region altogether.
Discussion: Pre-ERCP, treatment for choledocholithiasis included anastomosis between the common hepatic duct or proximal common bile duct and duodenum with a distal stump draining into the ampulla of Vater. Following the surgery air in the biliary tree acted as the sole indication of functional anastomosis. However, 5-10 years after the procedure, these patients sometimes presented with ascending cholangitis. This phenomenon of the development of stones and subclinical or clinical infection is known as Sump syndrome. The distal duct draining into the ampulla of Vater acts as a recess where static bile and debris keep accumulating, acting as a home for bacterial proliferation. This generally leads to pancreatitis or recurrent cholangitis. For imaging, an ultrasonogram may reveal stones and ductal dilation which might hint at the diagnosis. Finally, ERCP is both diagnostic and therapeutic with sphincterotomy and endoscopic removal. Adequate antibiotic coverage is necessary. Surgical Roux-en-y hepaticojejunostomy proves to be a definitive treatment if the patient requires multiple ERCPs.

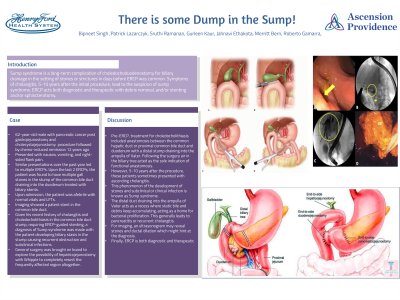
Figure: Obstructed Stent upon ERCP
Disclosures:
Bipneet Singh indicated no relevant financial relationships.
Patrick Lazarczyk indicated no relevant financial relationships.
Sruthi Ramanan indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Jahnavi Ethakota indicated no relevant financial relationships.
Merritt Bern indicated no relevant financial relationships.
Roberto Gamarra indicated no relevant financial relationships.
Bipneet Singh, MD1, Patrick Lazarczyk, DO2, Sruthi Ramanan, MD1, Gurleen Kaur, MD3, Jahnavi Ethakota, MD1, Merritt Bern, MD1, Roberto Gamarra, MD4. P0121 - There is Some Dump in the Sump, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
